- Health
Vaccines, treatments reduced public health threat posed by COVID-19, explaining different approach in 2024 compared to 2020
Key takeaway
The combination of vaccination, better treatments, widespread population immunity, and the emergence of SARS-CoV-2 variants mean that COVID-19 patients now experience milder disease and are less likely to die. These improvements have reduced the immediate public health risk posed by COVID-19, explaining a change in guidelines.
Reviewed content
Verdict:
Claim:
COVID-19 has been like the flu since the beginning of the pandemic
Verdict detail
Lack of context: The claim overlooks the fact that many things changed between 2020 and 2024. These changes explain why the CDC chose to update its guidelines and use a unified approach toward respiratory diseases including both the flu and COVID-19. Several factors that weren’t at play in the first years of the pandemic, including vaccination, virus variants, and better treatments, have since turned COVID-19 into a disease that is often milder than it was in the acute phase of the pandemic.
Full Claim
COVID-19 has been like the flu since the beginning of the pandemic; We should always have treated COVID-19 like the flu; people equating COVID-19 with the flu in 2020 or 2021 were right
Review
The U.S. Centers for Disease Control and Prevention (CDC) released updated guidelines for protection against respiratory diseases on 1 March 2024. Respiratory diseases include the flu, respiratory syncytial virus (RSV), and, for the first time, COVID-19.
These guidelines summarized precautions that most people are familiar with four years after the COVID-19 pandemic began. For instance, the CDC recommended that people cover their nose and mouth when sneezing and coughing, wash their hands, wear a mask and avoid close contact when sick, and incorporate fresh air into crowded, indoor spaces when possible.
One notable change in the guidelines was that people with symptoms matching COVID-19 may not need to remain isolated for five days anymore. Instead, the CDC recommends that people remain isolated until 24 hours after both their symptoms get better overall and they no longer have a fever.
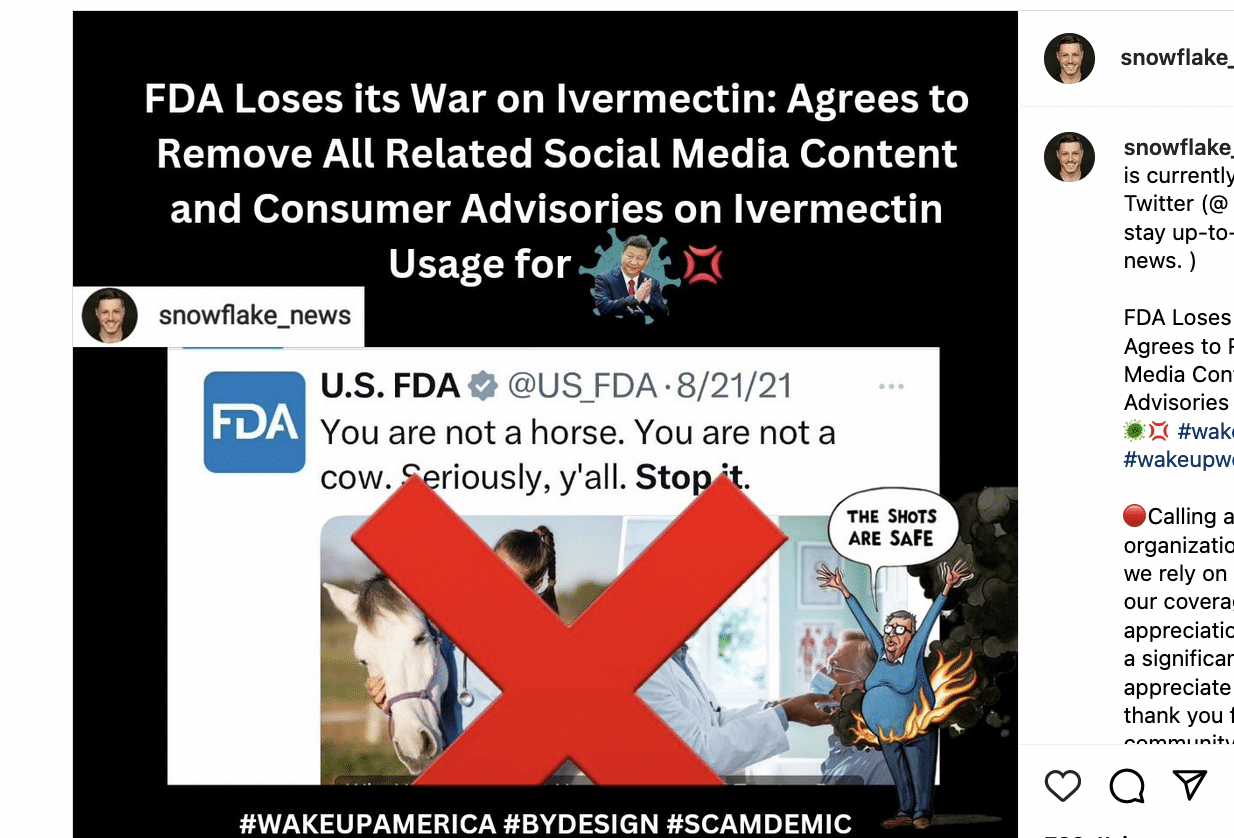
As mentioned above, these guidelines apply to all kinds of respiratory diseases, flu and COVID-19 alike. This prompted some people to claim that those who compared COVID-19 to the flu a few years ago, including former president Donald Trump, were right all along.
For instance, this Instagram post placed two headlines side by side. One is from October 2020 and stated that Facebook had removed a post from Trump equating COVID-19 with the flu. The other is from a March 2024 article in the Wall Street Journal reacting to the change in CDC guidelines stating that we can “treat Covid like the flu now”.
As the post’s comments illustrate, the post implies that we should always have treated COVID-19 like the flu, that COVID-19 is just another winter illness, and that those who made this claim at the beginning of the pandemic were right.
However, this interpretation of the updated CDC guidelines and media headlines is misleading. Indeed, it doesn’t take into consideration that many aspects of the COVID-19 situation changed over time, which prompted the CDC to change its optics on COVID-19. We provide details below.
The severity of COVID-19 decreased over time
The CDC’s decision to update and simplify guidelines for COVID-19 and other respiratory diseases is based on the fact that the epidemiological situation relating to COVID-19 significantly improved when comparing 2022 and 2023 to the first years of the pandemic in 2020 and 2021.
“CDC is making updates to the recommendations now because the U.S. is seeing far fewer hospitalizations and deaths associated with COVID-19 and because we have more tools than ever to combat flu, COVID, and RSV.”, the CDC said in a press release.
At the beginning of the pandemic, COVID-19 became the third leading cause of death in the U.S. It resulted in more than 800,000 excess deaths in 2020 and 2021, according to an analysis from the CDC dataset for “National and State Estimates of Excess Deaths“. Numerous reports documented the shortage of beds in hospitals and intensive care units owing to the influx of COVID-19 patients.
Thus, comparing COVID-19 and the flu was misleading back then, as the threat of both diseases to public health was conspicuously different. Furthermore, equating both diseases could create a false sense of security and undermine the efforts of the population and the authorities to curb the spread of COVID-19.
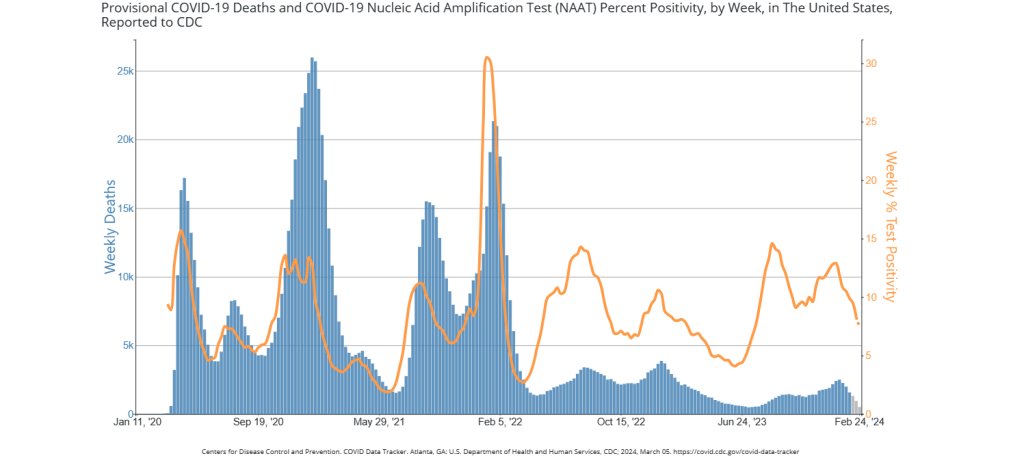
Later on, however, the situation began to ease. The CDC data showed that the number of weekly COVID-19 deaths (Figure 1) and hospitalizations significantly decreased from the 2020-2021 period to the 2022-2023 period.
At the same time, the positivity—the percentage of positive COVID-19 tests—remained similar over the years. This indicated that even though people still became infected, the outcomes were less severe compared to the first years of the pandemic.
The CDC also noted that COVID-19 dropped from the third leading cause of death in 2020 and 2021 to tenth in 2023.
The CDC also reported that multisystem inflammatory syndrome in children (MIS-C), a rare but severe condition associated with COVID-19 in children, became less frequent in 2022 and 2023 compared to 2020 and 2021.
Furthermore, physicians and infectious diseases scientists observed that COVID-19 patients increasingly presented symptoms of upper respiratory tract infection, instead of lower respiratory tract infection, which was the case at the beginning of the pandemic.
Upper respiratory tract infections are generally milder, characterized by sore throat and runny nose, whereas lower respiratory tract infections tend to be more severe. Consistently, a study found that COVID-19 patients with only upper respiratory symptoms had better clinical outcomes than patients with lower respiratory symptoms[1]. In short, COVID-19 is now more likely to produce milder disease.
In other words, while COVID-19 posed a great and urgent threat to public health in 2020 and 2021, the risk of severe disease has decreased over the years. The CDC made clear that this doesn’t mean that COVID-19 and the flu are now the same and that COVID-19 still bears significant risks for more vulnerable groups like babies and the elderly. But the improvement of the epidemiological situation in 2022 and 2023 led the agency to consider COVID-19 as a serious respiratory disease that can be handled similarly to other respiratory infections like the flu.
Widespread immunity, new variants, better treatments explain the reduced public health threat posed by COVID-19
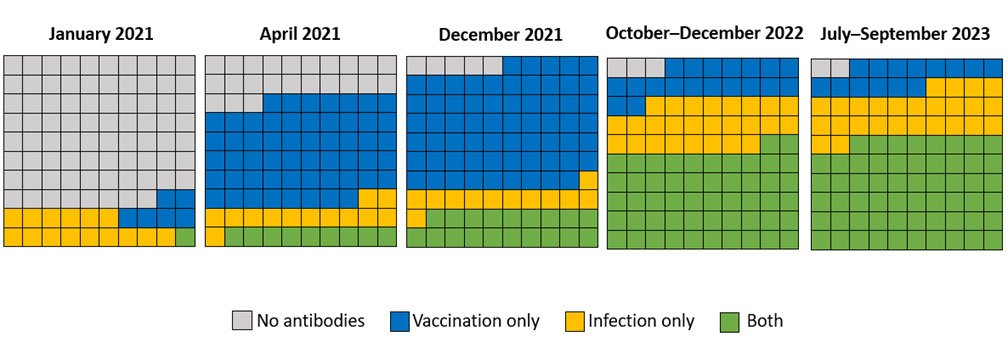
There are several drivers behind the improvement of the epidemiological situation. First, a large majority of the population now has some level of immunity against SARS-CoV-2, compared to the first couple of years of the pandemic (Figure 2).
At the beginning of the pandemic, SARS-CoV-2 was a new virus against which people had no immunity. In other words, our bodies were largely defenseless against it.
However, this situation has evolved over time. Vaccines became available in December 2020, and more and more people got progressively vaccinated against the virus. Along the way, more and more people who got COVID-19 recovered.
Both developments—mass vaccination and many people getting infected and recovering—generated widespread immunity among the population, as the CDC explained in its updated guidance.
While the seroprevalence—the proportion of the population with antibodies against SARS-CoV-2— was only 22% in 2021, it reached 98% by the end of 2023. Having antibodies against the virus doesn’t necessarily prevent all infections, but it reduces the risk of developing severe disease.
Second, the virus itself changed. Since January 2022, the Omicron variant and its subvariants, including the predominant variant circulating as of March 2024, has since superseded older variants of the virus such as Alpha or Delta[2].
Omicron infections are generally associated with milder symptoms than the previous variants, because this variant is more likely to infect from the lower respiratory tract than the upper respiratory tract. As explained earlier, upper respiratory symptoms are usually less severe because the lungs don’t suffer as much damage.
Finally, the U.S. Food and Drug Administration (FDA) approved Paxlovid, an oral treatment against mild to severe COVID-19, in March 2023. Studies showed that Paxlovid significantly reduced the risk of death and hospitalization among COVID-19 patients[3], making it an effective tool in the fight against the disease.
Conclusion
The implication that COVID-19 should always have been treated as the flu because of the CDC’s recent update to COVID-19 guidelines is misleading. This fails to take into account the very different level of risk that COVID-19 posed to the public at the beginning of the pandemic relative to now.
The combination of better COVID-19 treatments, widespread vaccine- and infection-induced immunity of the general population, and SARS-CoV-2 variants, have significantly reduced the immediate public health threat posed by COVID-19. Although the disease can still be severe and shouldn’t be taken lightly, people are now less likely to die from COVID-19 and more likely to develop mild disease than they did during the initial years of the pandemic.
These statistics indicate that COVID-19 now poses less of an immediate public health threat than it did in 2020, which is why the CDC decided to update COVID-19 guidelines and merge it with guidelines for other respiratory diseases like the flu.
REFERENCE
- 1 – Nakagawara et al. (2022) Impact of upper and lower respiratory symptoms on COVID-19 outcomes: a multicenter retrospective cohort study. Respiratory Research.
- 2 – Lambrou et al. (2022) Genomic Surveillance for SARS-CoV-2 Variants: Predominance of the Delta (B.1.617.2) and Omicron (B.1.1.529) Variants — United States, June 2021–January 2022. Morbidity and Mortality Weekly Report.
- 3 – Amani B. (2022) Efficacy and safety of nirmatrelvir/ritonavir (Paxlovid) for COVID-19: A rapid review and meta-analysis. Journal of medical virology.