- Health
Sperm washing to help HIV-discordant couples conceive biological children safely was reported in the 90s; not “huge medical breakthrough” in 2022
Key takeaway
Sperm washing is a general technique used in assisted reproductive technology, as it is helpful in obtaining healthy, motile sperm samples to be used later for in vitro fertilization or intrauterine insemination. But it has also become a useful procedure for helping HIV-discordant couples—where one partner is HIV-positive while the other is HIV-negative—to conceive biological children more safely by removing semen components that carry high amounts of the virus.
Reviewed content
Verdict detail
Misleading: Sperm washing to minimize HIV viral load in sperm samples for intrauterine insemination and in vitro fertilization was first reported in 1992 by a team of researchers from Italy. It’s now a common procedure used in assisted reproductive technology to help HIV-discordant couples conceive biological children more safely. While Moatshe confirmed that she performs this procedure as part of her work as an embryologist, it wasn’t “a huge medical breakthrough” only achieved in 2022 as the post suggested.
Full Claim
“Meet Lebo Moatshe from South Africa who successfully removed HIV from a sperm cell in a lab which is a huge medical breakthrough”
Review
A post published by the Facebook page Africa is HOME in late May 2022 claimed that a scientist named Lebo Moatshe from South Africa achieved “a huge medical breakthrough” by “successfully removing HIV from a sperm cell”. Curiously, the post also contained a link directing users to a post encouraging them to sign up for a free bank account. There were other Facebook and Instagram posts that also shared the same information, although without the link (see examples here and here).
However, posts like these led to misunderstanding by users who interpreted the posts to mean that Moatshe is the first person to accomplish this feat. In fact, the technique was pioneered by a team of researchers in Italy, led by obstetrician and gynecologist Augusto Enrico Sempini. Their work on sperm washing of samples from HIV-positive men was already published in 1992 in the medical journal The Lancet[1]. Sempini and other scientists continued to follow up on this work, as evidenced by later published studies[2,3].
Indeed, the misunderstanding later led Moatshe, who is an embryologist, to correct the record on Twitter, clarifying that she wasn’t the first person to perform this procedure of sperm washing: “It has been done by many over a period of years. It is a common thing in reproductive biology. I have just acquired the skill recently as an intern hence my post.”
Hi Mimi. Thank you for sharing, however, I must clarify that I’m not the first person to do this procedure. It has been done by many over a period of years. It is a common thing in reproductive biology. I have just acquired the skill recently as an intern hence my post. 🌸
— Moatshe ✨🌸 (@Lebzito_xo) May 28, 2022
Sperm washing is a general technique used in assisted reproductive technology, as it is helpful in obtaining healthy, motile sperm samples for in vitro fertilization or intrauterine insemination. In fact, it is a standard procedure for couples undergoing fertility treatment.
But it has also become a useful procedure for helping HIV-discordant couples—where one partner is HIV-positive while the other is HIV-negative—conceive biological children more safely. Before the technique of sperm washing was applied in such cases, a HIV-positive man and a HIV-negative woman who wished to have their own children ran a strong risk of virus transmission during sexual intercourse. Indeed, in 1988, the U.S. Centers for Disease Control and Prevention (CDC) discouraged insemination using sperm samples from HIV-positive men[4]. Condoms are highly effective at protecting against HIV infection, but obviously cannot be used if the couple wishes to conceive.
HIV is transmitted through body fluids like blood and semen. Semen comprises sperm cells and fluid. The fluid contains a mixture of sugars, amino acids, citric acid, minerals, and hormones. These help sperm cells to stay viable and motile. Semen also contains lymphocytes, a type of white blood cell, which are among the targets of HIV infection. A study by Sempini et al. reported that lymphocytes carry the largest load of HIV in the semen[1,5].
Sperm washing separates the sperm cells from the rest of semen, which minimizes the viral load that the uninfected partner will be exposed to. In order to do this, scientists use a combination of gradient centrifugation, washing, and the swim-up procedure. Centrifugation uses centrifugal force to separate particles in a liquid based on their density. This results in a pellet of sperm cells at the bottom of the container; the upper portion comprises liquid that contains the potentially infected lymphocytes, which can be discarded while retaining the sperm cells. The cells are then washed. Finally, the swim-up procedure allows scientists to isolate motile sperm, as these will swim to the upper portion of the liquid. The sperm samples can be used later in intrauterine insemination or in vitro fertilization (see diagram below by Sempini et al.).
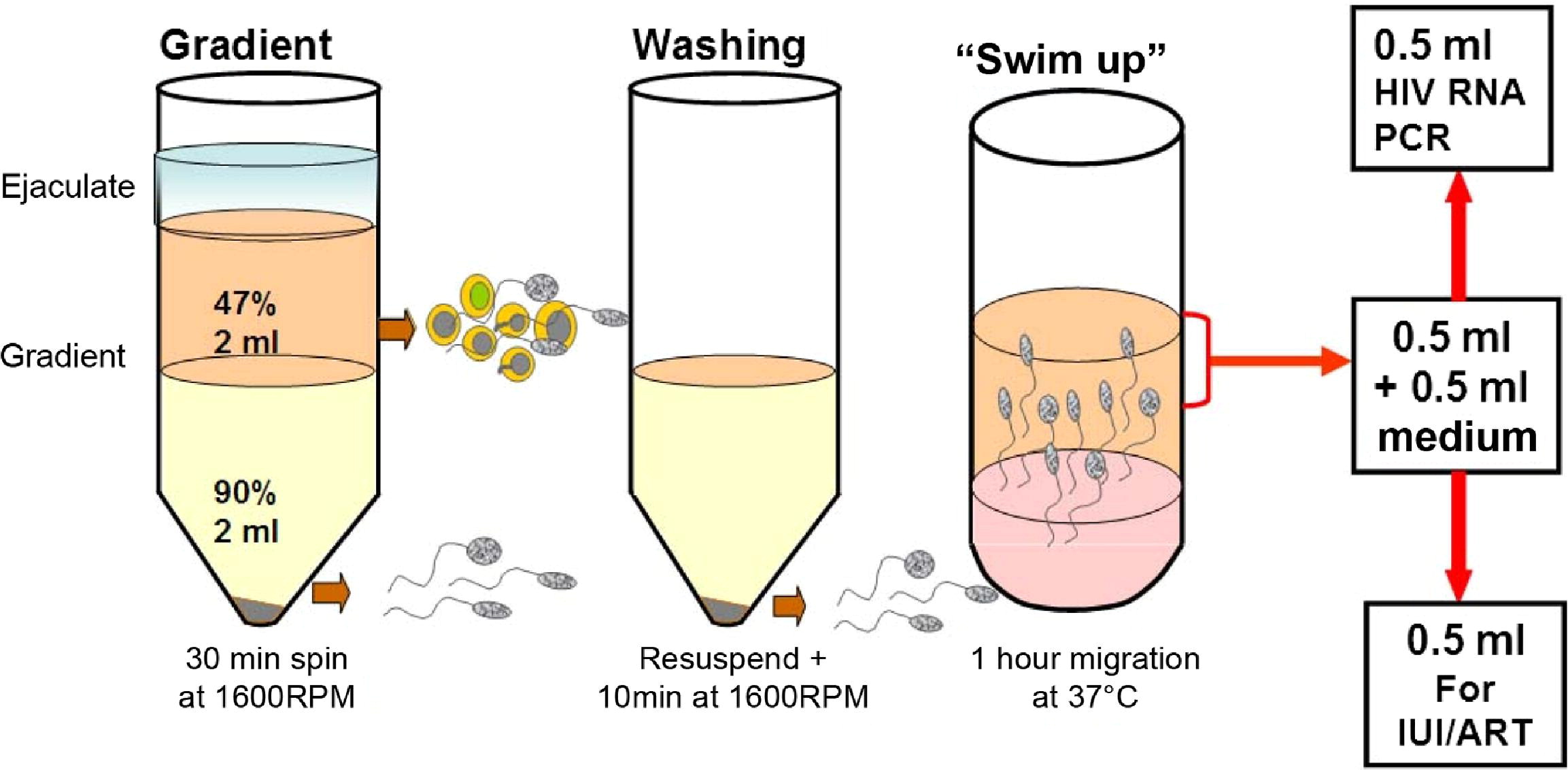
Steps involved in sperm washing, illustrated in a study by Sempini et al[2]. IUI: intrauterine insemination, ART: assisted reproductive technology, RPM: revolutions per minute (denoting centrifuge speed to be used).
As an additional safety measure, part of the final sperm sample would be tested for HIV using PCR. A washed sperm sample that tests positive for HIV would be discarded.
There are also other safety measures that a HIV-discordant couple can take to further minimize the risk of transmission while trying to conceive, apart from sperm washing. For example, the HIV-positive partner can take antiretroviral therapy, which stops HIV from replicating, while the HIV-negative partner would use preexposure prophylaxis (PrEP) to reduce their risk of infection.
Although the CDC stated in 1990 that “no data exist to support the safety of any procedure purported to remove HIV from semen”, scientific developments since that time have led the CDC to reverse its stance. In a 2017 Morbidity and Mortality Weekly Report[5], researchers wrote:
REFERENCES
- 1 – Sempini et al. (1992) Insemination of HIV-negative women with processed semen of HIV-positive partners. The Lancet.
- 2 – Sempini et al. (2013) Safe conception for HIV-discordant couples: insemination with processed semen from the HIV-infected partner. American Journal of Obstetrics and Gynecology.
- 3 – Zafer et al. (2015) Effectiveness of semen washing to prevent human immunodeficiency virus (HIV) transmission and assist pregnancy in HIV-discordant couples: a systematic review and meta-analysis. Fertility and Sterility.
- 4 – U.S. Centers for Disease Control and Prevention. (1988) Semen banking, organ and tissue transplantation, and HIV antibody testing. Morbidity and Mortality Weekly Report.
- 5 – Kawwass et al. (2017) Strategies for Preventing HIV Infection Among HIV-Uninfected Women Attempting Conception with HIV-Infected Men — United States. Morbidity and Mortality Weekly Report.