- Health
Methodologically flawed cholesterol study from 2016 used to support false claims that high cholesterol increases longevity
Key takeaway
High levels of cholesterol in the blood is a major risk factor for developing heart disease, which is the leading cause of death in the U.S. and globally. Therefore, regularly checking cholesterol levels is an important first step in reducing the risk of developing or dying from heart disease and stroke. Even small decreases in blood cholesterol can significantly reduce the risk, something that can be achieved through a balanced diet, physical activity, and medication.
Reviewed content
Verdict:
Claim:
“A new study found that 92 percent of people with a high cholesterol level lived longer”
Verdict detail
Inadequate support: The study on which this claim is based has multiple methodological issues and potential biases that make its results and conclusions unreliable.
Cherry-picking: The claim that high cholesterol makes you live longer relies on a single, flawed study and ignores ample evidence from clinical trials showing that lowering cholesterol levels reduces the risk of death.
Full Claim
“A new study found that 92 percent of people with a high cholesterol level lived longer”
Review
On 11 March 2023, a Facebook post claimed, “A new study found that 92 percent of people with a high cholesterol level lived longer”. The post linked to an article with that exact title published on Livingtraditionally.com in 2020, which in turn cited a study by Ravnskov et al. published in BMJ Open in 2016[1].
This study analyzed cholesterol and all-cause mortality data from 19 previous studies involving 68,094 participants aged 60 and older, concluding that 92% of the people with high “bad” cholesterol levels lived longer than those with lower levels. Based on these results, the authors called for “a re-evaluation of the guidelines for cardiovascular prevention, in particular because the benefits from statin treatment have been exaggerated”.
These results contradicted the generally accepted lipid hypothesis, which states that elevated blood cholesterol leads to heart disease, triggering claims that cholesterol levels are unrelated to heart disease and that statins—a medication that lowers blood cholesterol levels—might be useless. However, as we explain in detail below, experts have warned that such claims are unsupported because the study had serious flaws and potential biases that called its results into question.
What is “good” and “bad” cholesterol?
Cholesterol is a fatty molecule that circulates in the blood and is essential for making cell membranes, hormones, and vitamin D. The liver produces most of the cholesterol that the body needs. The remaining cholesterol comes through food from animal sources such as egg yolks, meat, and dairy products, sometimes in excessive amounts.
Fats like cholesterol can’t travel alone in a water-based liquid as the blood. But they can be combined with proteins to form two main types of lipoproteins that can move around the bloodstream more easily. The so-called “bad” cholesterol refers to the low-density lipoprotein (LDL), which is sticky and can progressively accumulate in fatty deposits called plaques inside the blood vessels (Figure 1). This condition called atherosclerosis may cause the vessels to become too narrow, which impairs blood flow and increases the risk of heart disease.
In contrast, the high-density lipoprotein (HDL) is often referred to as “good” cholesterol because it carries the LDL cholesterol (LDL-C) from the bloodstrem back to the liver to eliminate it from the body. Thus, it reduces the risk of heart disease (Figure 1).
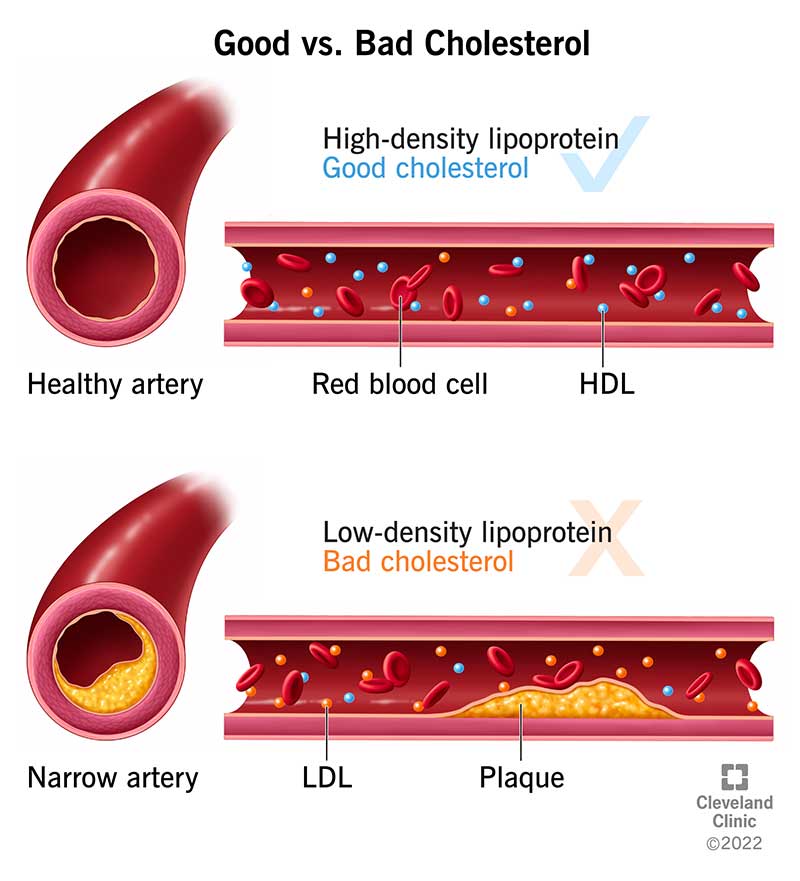
Figure 1. Effect of high-density lipoprotein (HDL) (“good” cholesterol, up) and low-density lipoprotein (“bad” cholesterol, bottom) in the blood vessels. LDL contributes to plaque formation, while HDL helps remove blood cholesterol. Source: Cleveland Clinic.
The analysis by Ravnskov et al. showed signs of cherry-picking
The study’s findings were widely covered in the media at the time it was published in 2016, prompting the British Heart Foundation to publish a cautionary article pointing out multiple flaws and methodological limitations of the study. Colin Baigent, a professor of epidemiology at the University of Oxford, told the U.K. Science Media Centre that the study had “a number of serious weaknesses and, as a consequence, has reached completely the wrong conclusion”.
One of the main criticisms involved the selection of the 19 individual studies included in the analysis. Briefly, the authors searched PubMed—a biomedical literature database maintained by the U.S. National Institutes of Health—for studies in English containing the words “lipoprotein AND (old OR elderly) AND mortality NOT animal NOT trial“. Among them, the authors selected those studies “where the title or abstract indicated that they might include LDL-C data of elderly people”.
The BHF explained that this search “may have excluded studies that evaluated LDL-C as a risk factor for death if the study did not mention it in the title or abstract”. Likewise, the Centre for Evidence-Based Medicine (CEMB) at the University of Oxford pointed out in a detailed response to the study that such a narrow search with so few keywords presented “a high risk of bias for missing important and relevant studies”.
Tim Chico, a professor of cardiovascular medicine at the University of Sheffield, told the Science Media Centre that the analysis by Ravnskov et al. indeed left out relevant clinical trials:
“There have been several studies that tested whether higher cholesterol increases the risk of heart disease, by lowering cholesterol in elderly patients and observing whether this reduces their risk of heart disease (for example the PROSPER study). These have shown that lowering cholesterol using a drug does reduce the risk of heart disease in the elderly, and I find this more compelling than the data in the current study. I am surprised the authors of this study do not refer to such trials, which tends to make their own paper disappointingly unbalanced.”
In addition, the CEMB explained that the search produced 282 studies, 263 of which were excluded without providing specific reasons for these exclusions. In fact, the CEMB found inconsistencies in the inclusion and exclusion criteria. For example, the authors excluded a 2015 study by Postmus et al. that found associations between genetic predisposition to high LDL-C and higher mortality even though it matched the selection criteria[2].
In contrast, the authors included a study by Bathum et al. where it’s unclear whether the study should have been included based on the authors’ inclusion and exclusion criteria, according to the CEBM response[3]. Specifically, the authors stated they excluded “studies without multivariate correction for the association between LDL-C and all-cause and/or CV mortality”. Multivariate correction is a statistical method that corrects for multiple potential confounding factors, which are variables other than the ones being studied that also affect the measured outcome. Table 2 in Ravnskov et al. listed all the specific variables that were accounted for in each study. However, in the study by Bathum et al. the table simply stated, “Cox regression analysis. No details” (Figure 2).
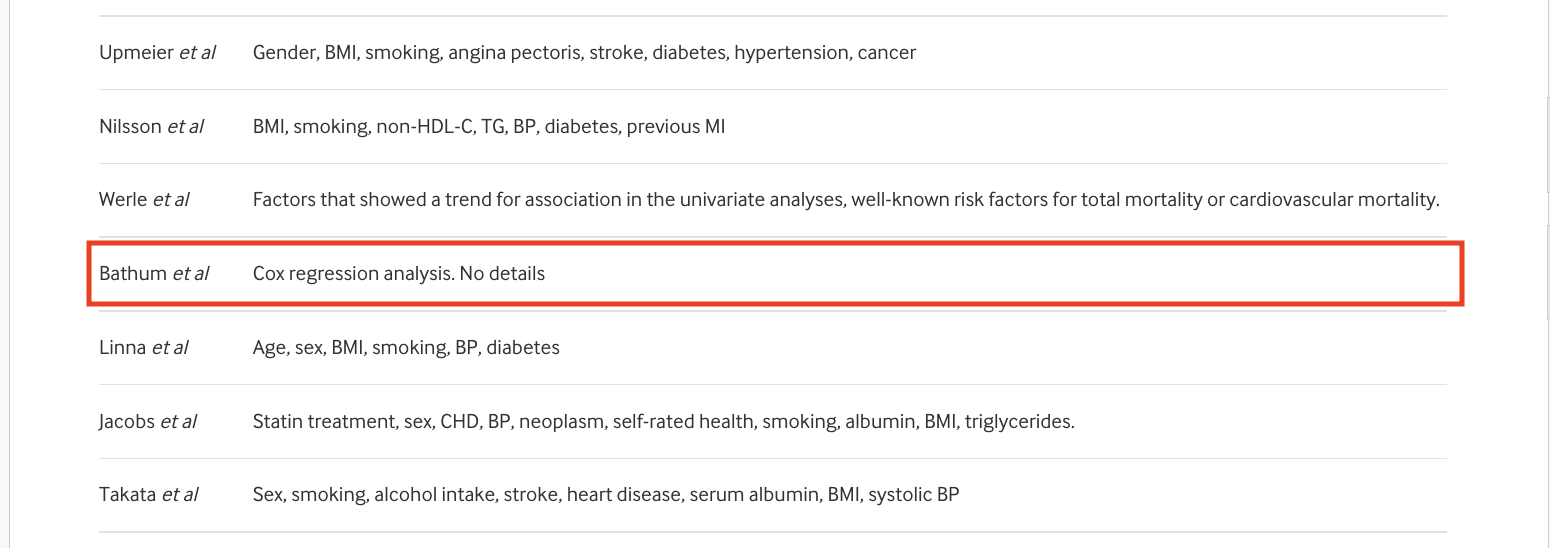
Figure 2. Detail from Table 2 from Ravnskov et al.[1] showing the factors corrected for in the multivariate correction of each study. The study by Bathum et al. is highlighted with a red square.
While Cox regression is a type of multivariate correction, the lack of detail about the variables corrected in this study contrasts with the greater level of detail provided for other studies. This raises questions about whether the study by Bathum et al. adequately met the authors’ inclusion criteria, as the lack of information makes ascertaining this impossible.
This study, which accounted for more than 65% of the total number of participants in the analysis by Ravnskov et al., found an association between higher cholesterol levels and lower all-cause mortality in people aged 50 and older. However, the study still showed that statin treatment improved survival “in almost all age and lipoprotein/triglyceride groups”. Since this study accounted for most of the data analyzed by Ravnskov et al., their assertion that “the benefits from statin treatment have been exaggerated” lacks support.
All these issues suggest potential cherry-picking in the studies analyzed. It is important to note that several authors of the study, including the first author Uffe Ravnskov, had previously questioned the association between LDL-C and heart disease or the use of statins. One of them is cardiologist Aseem Malhotra, who had previously criticized statin treatment and has since become well-known for spreading misleading claims about COVID-19 vaccine safety.
The study didn’t take into account other factors that might impact mortality
Another critical issue in the study is that the authors didn’t account for important factors that can confound the association between LDL-C and mortality, including statin treatment. Not accounting for such factors can mask an association between the two variables or falsely suggest an association when there is none.
For obvious reasons, people with high LDL-C levels are much more likely to be prescribed statins or lifestyle changes such as a healthier diet or more physical activity than those with low LDL-C levels. Ravnskov et al. acknowledged that “some participants with high LDL-C may have started statin treatment during the observations period”. However, the study didn’t take into account the potential effect of this treatment on mortality.
According to the CEBM, the lack of control for these confounding factors represents a “major bias and more likely underpins the majority of the observed inverse associations”.
The study had additional methodological problems. For example, only nine of the 19 individual studies analyzed actually included deaths from cardiovascular disease, which is the cause of death primarily related to cholesterol levels. The study also didn’t indicate the quality or the level of certainty of the data included in the analysis.
Based on these limitations, John Danesh, BHF professor of epidemiology and medicine at the University of Cambridge told the U.K. Science Media Centre:
“Because Ravnskov and colleagues used crude study methods, we cannot trust the statistical correlations they have reported between cholesterol levels and cardiovascular disease risk. For example, because their analysis lacked access to data on each participant included in their analysis, they relied on limited, aggregated and inconsistent information from published sources, an approach liable to bias.”
Evidence from clinical trials show that lowering cholesterol levels reduces the risk of death
Since Carl Mueller first reported a link between blood cholesterol levels in humans and heart disease in 1938, the lipid hypothesis has been extensively debated[4]. The reason for the controversy was that initial studies were mostly studies in animals that weren’t representative of the way the human body processes cholesterol or epidemiological studies that weren’t conclusive about whether cholesterol levels were causally related with heart disease.
But cardiologist Christopher Labos debunked in a post for Science-Based Medicine the most common criticisms against the lipid hypothesis and explained that the controversies “belong to a different time”, when we didn’t have as much information about cholesterol and its effect on human health as we do now.
Although the science has moved on with time, the same objections to the lipid hypothesis persist, which could have negative effects on people’s health. Denying the impact of cholesterol levels on heart disease is dangerous in two different ways. First, it might encourage people to eat more animal fats, increasing their risk of heart disease.
Second, it implies that medication for lowering cholesterol levels such as statins isn’t necessary or might do more harm than good. These narratives can impact a patient’s outcome. For example, a study suggested that negative statin-related news might be associated with people discontinuing their statin treatment and an increased risk of heart attack and death from cardiovascular disease[5].
While other risk factors such as smoking, obesity, and diabetes increase the risk of heart disease, evidence from three decades of epidemiologic, genetic, and clinical studies clearly show that lowering cholesterol levels reduces cardiovascular and all-cause mortality. One of the first clinical trials demonstrating this association was published in the Lancet in 1994[6]. This study showed that long-term treatment with statins lowered LDL-C levels by 35%, which improved survival in patients with coronary heart disease.
The results of larger and more comprehensive analyses than that of Ravnskov et al. also contradict this study’s conclusions. For example, a 2010 meta-analysis using individual data from 170,000 participants in 26 randomized trials found that further reductions in the levels of LDL-C in blood was associated with further reductions in the annual rate of cardiovascular disease[7].
More recently, a 2016 evidence report and systematic review by the U.S. Preventive Services Task Force found that lowering LDL-C levels with statins reduced mortality due to cardiovascular disease and all-cause mortality[8]. The review didn’t find evidence of serious adverse reactions to the medication, in agreement with a 2023 evaluation by the U.K. National Institute for Health and Care Excellence (NICE), which concluded that statins are safe to use by a much broader range of people than initially thought. The guideline draft for consultation can be read here.
As Jeremy Pearson, a former associate medical director at the BHF, summarized:
“[T]he evidence from large clinical trials demonstrates very clearly that lowering LDL cholesterol reduces our risk of death overall and from heart attacks and strokes, regardless of age. There is nothing in the current paper to support the authors’ suggestions that the studies they reviewed cast doubt on the idea that LDL cholesterol is a major cause of heart disease or that guidelines on LDL reduction in the elderly need re-evaluating.”
REFERENCES
- 1 – Ravnskov et al. (2016) Lack of an association or an inverse association between low-density-lipoprotein cholesterol and mortality in the elderly: a systematic review. BMJ Open.
- 2 – Postmus et al. (2015) LDL cholesterol still a problem in old age? A Mendelian randomization study. International Journal of Epidemiology.
- 3 – Bathum et al. (2012) Association of lipoprotein levels with mortality in subjects aged 50 + without previous diabetes or cardiovascular disease: A population-based register study. Scandinavian Journal of Primary Health Care.
- 4 – Mueller (1938) Xanthomata, Hypercholesterolemia, Angina Pectoris. Acta Medica Scandinavica.
- 5 – Nielsen & Nordestgaard (2016) Negative statin-related news stories decrease statin persistence and increase myocardial infarction and cardiovascular mortality: a nationwide prospective cohort study. European Heart Journal.
- 6 – Scandinavian Simvastatin Study Group (1994) Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). The Lancet.
- 7 – Cholesterol Treatment Trialists’ (CTT) Collaboration (2010) Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170 000 participants in 26 randomised trials. The Lancet.
- 8 – Chou et al. (2016) Statins for Prevention of Cardiovascular Disease in Adults
Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA.