- Health
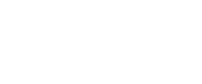
Internet memes based on hearsay claim that hospital laboratories falsify COVID-19 tests to inflate numbers without evidence
Key takeaway
There is no evidence that hospital laboratories have falsified the number of COVID-19 positives. While false-positives can occur, experts agree that they are a rare event. On the contrary, false-negatives are hard to control as they can be due to many different factors apart from test accuracy, including the type of specimen analyzed, the sample handling, or the stage of infection. Failing to correctly identify infected people would promote disease transmission and constitute a public health risk.
Reviewed content
Verdict detail
Unsupported: There is no evidence supporting the claim that hospitals have intentionally manipulated COVID-19 testing to increase the number of positive results. Each batch of samples follows rigorous laboratory controls, and testing results are routinely supervised by both human and computer systems.
Full Claim
U.S. hospital laboratories falsify COVID-19 tests to inflate the number of positive results ... Nurses sent unused swabs for COVID testing and they all came back positive
Review
This Facebook meme published on 27 June 2020 claims that a San Francisco hospital lab intentionally falsified COVID-19 tests to inflate the number of positive results. A British actor, Robert Tayman, tweeted on 29 June a version of this claim and afterwards asserted in the Twitter thread that the nurses worked in “a major hospital in Baltimore”. Both tweets were deleted two days later, but screenshots of the tweets continue to circulate. The claim has been shared in different forms thousands of times and viewed by more than a million people through Facebook, Instagram, and Twitter.
Since the beginning of the COVID-19 pandemic, testing has emerged as a key strategy to slow the spread of the virus, together with other measures including frequent hand-washing, use of masks, and physical distancing1. With several countries beginning to reopen, the identification and isolation of infected individuals and their close contacts can help to prevent transmission and reduce the impact of COVID-19 on healthcare systems.
There are mainly two types of COVID-19 tests serving for different purposes. Antibody or serological tests can detect the immune response against the virus and are used to identify past infections. Viral tests can detect the presence of either the nucleic acid (typically by polymerase chain reaction or PCR) or specific viral proteins in samples taken from the respiratory tract, such as nasal swabs, and enable the identification of currently infected individuals for their isolation and treatment.
Crucial aspects of diagnostic testing are specificity and sensitivity, which are respectively defined as the rate of false positives and false negatives that a test produces. Since February, the U.S. Food and Drug Administration (FDA) has approved the emergency use of 138 diagnostic tests for COVID-19 and established in its testing policy a minimum accuracy of 95%. But the diagnostic capacity of these tests depends as well on other factors, including the quality and handling of the samples, the type of sample used2, and the stage of infection.
While diagnostic COVID-19 tests may indeed produce false-positive results, experts consider this rate very low and less concerning than false negatives. False positives may force the person to take unnecessary precautions, but false negatives can increase the spreading of the virus. Michael Mina, assistant professor of epidemiology and a faculty member in the Center for Communicable Disease Dynamics of the Harvard T.H. Chan School of Public Health, explained in an 8 June press conference at Harvard that “I’m less concerned about false positives”, but “false negatives are a more difficult thing to tease out”.
According to data from the U.S. Centers for Disease Control and Prevention (CDC), the average rate of COVID-19 positive results is 9%, although it varies for each state. Anomalous deviations from the expected rate in a laboratory are verified by a re-analysis of the samples. As Mina remarked, “it is important to continuously do quality controls on your methods”. Fyodor Urnov, head of the SARS-CoV-2 clinical diagnostic laboratory at the University of California, Berkeley, explained that there are “rigorous in-process controls for every batch of specimens we test and provide the results for, and should these controls fail, we repeat the test”.
There is indeed one case where several nurses filed a lawsuit against a hospital in Georgia for allegedly falsifying COVID-19 negative, not positive, results to cover up a COVID-19 outbreak. However, Urnov explained that the test results are analyzed and reported by “a computer system, not a human being”. While “a clinical laboratory scientist reviews the results reported by the computer, they cannot change them”.
In summary, the claim that hospitals intentionally manipulated COVID-19 testing results is not supported by evidence, nor supported by trustworthy sources. The original source of the claim could not provide any evidence to substantiate the claim but explained to PolitiFact that it was a “word-of-mouth story” from his mother. COVID-19 diagnostic testing follows rigorous laboratory controls and continuous supervision by qualified personnel as well as computer systems.
Scientists’ Feedback

Professor, Innovative Genomics Institute, Berkeley, CA, USA
The false-positive rate of the test we are using, which is highly similar to the one used by the majority of such testing laboratories, is negligible (it is as close to zero as technically possible). We have rigorous in-process controls for every batch of specimens we test and provide the results for, and should these controls fail, we repeat the test. Further, and following standard practice, we have a computer system – not a human being – that analyses the test results and reports on each patient specimen. There is human oversight over the process: as specified by Federal and State laws, a dedicated professional, known as a clinical laboratory scientist (CLS), reviews the results reported by the computer, but cannot change them.
READ MORE
This claim has been also found unsupported by LeadStories. The specificity of COVID-19 diagnostic tests has been previously addressed in this review by Health Feedback.
REFERENCES
- 1 – Cheng et al. (2020) Diagnostic Testing for Severe Acute Respiratory Syndrome–Related Coronavirus 2. Annals of Internal Medicine.
- 2 – Yang et al. (2020) Evaluating the accuracy of different respiratory specimens in the laboratory diagnosis and monitoring the viral shedding of 2019-nCoV infections. medRxiv