- Health
Infectious diseases are caused by microorganisms; other factors may determine an individual’s susceptibility to infection, but the microorganism is still the cause
Key takeaway
Factors like nutrition, genetics and age can influence an individual’s susceptibility to a microorganism, such as a virus or a bacteria. These factors make individuals more or less likely to develop infections after they were exposed to a microorganism. That being said, even individuals who are young and healthy can develop infectious diseases because the cause of infectious diseases is still the microorganism.
Reviewed content
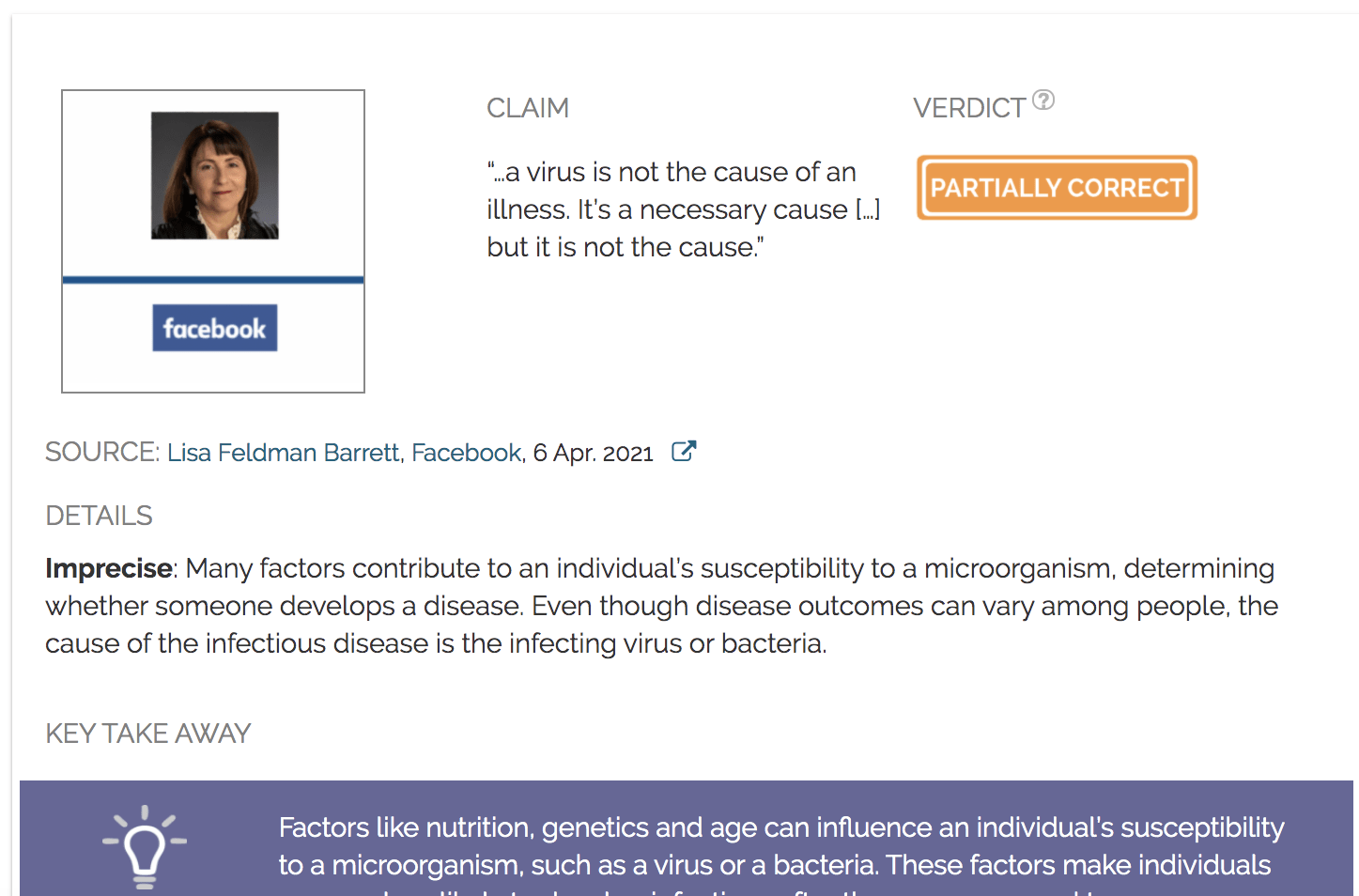
Verdict:
Claim:
“…a virus is not the cause of an illness. It’s a necessary cause […] but it is not the cause.”
Verdict detail
Imprecise: Many factors contribute to an individual’s susceptibility to a microorganism, determining whether someone develops a disease. Even though disease outcomes can vary among people, the cause of the infectious disease is the infecting pathogen.
Full Claim
“Exposure to a virus is not the same as infection […] That means that a virus is not the cause of an illness. It is a necessary cause. You can’t get a common cold without the virus. But it is not the cause.”
Review
The ongoing COVID-19 pandemic has made it clear that SARS-CoV-2 is not an equal-opportunity virus. Certain medical conditions, such as asthma, pregnancy, and diabetes among others, can make someone more likely to get severely ill from COVID-19 than those who don’t have these medical conditions. Additionally, people of low socio-economic status are more likely to be exposed to the virus, due to overcrowded living conditions and employment in jobs that don’t allow them to work from home[1].
Multiple scientific studies established that SARS-CoV-2 is the virus that causes COVID-19, as demonstrated in this Health Feedback review. Although the cause of COVID-19 is the same for everyone, various medical conditions can increase someone’s likelihood of catching the virus and how susceptible they are to serious illness and death. As detailed in another Health Feedback review, the majority of COVID-19 deaths occurred in people with pre-existing health conditions like diabetes and obesity.
On 6 April 2021, comedian Russel Brand posted a video on his Facebook page of him interviewing neuroscientist and psychologist Lisa Feldman Barrett, a professor at Northeastern University. In the video, Barrett argued that “a virus is not the cause of an illness”. She explained that though the viruses are a necessary cause because “you can’t get the common cold without the virus,” they are not the cause [Barrett’s emphasis]. The video received more than 390,000 views and more than 16,000 interactions on Facebook, including likes and comments.
As evidence, Barrett described experiments where scientists isolated human subjects in hotel rooms before exposing them to the same dose of one of the viruses that causes the common cold. According to Barrett, “only 20 to 40 percent, depending on the experiment, got sick with symptoms” and those who got sick had a history of chronic stress and childhood adversity. “What predicted who got sick was also the state of that person’s immune system, which is regulated by their brain,” Barrett said, before concluding that a person’s immune system and brain are also “necessary but not sufficient causes of illness”.
Barrett doesn’t provide a citation for the experiments, but a 1998 paper by Sheldon Cohen, a psychologist at Carnegie Mellon University who studies the connection between stress, immunity and disease, and his colleagues may be what Barrett was referring to in the video[2]. In the study, 276 volunteers completed a life stressor interview and received nasal drops containing a low infectious dose of a member of the rhinovirus family that cause more than half of cold-like illnesses[3]. The volunteers were kept in quarantine for the next five days, resulting in 40% of participants developing a cold.
The 1998 study showed that one type of stress was particularly linked to susceptibility to the rhinovirus: chronic stress. While stressful events lasting less than 1 month did not alter an individual’s susceptibility, chronic stress lasting at least one month did.
Barrett is right that work by Cohen and others demonstrated that stress has an impact on an individual’s susceptibility to infectious diseases. For example, stress is known to increase the level of a hormone called cortisol. In the long run, elevated cortisol levels can negatively impact the immune system’s ability to function properly[4].
Although people varied in their susceptibility to developing the disease, the rhinovirus was still the cause of participants’ cold symptoms in the study. Without receiving the nasal drop containing the rhinovirus, none of the patients would have developed a cold. When discussing the causes and outcomes of a disease, distinguishing between a “necessary cause” and “cause,” and describing chronic stress as a cause rather than a contributing factor, as Barrett did, is imprecise and potentially misleading.
Every infectious disease begins when someone comes into contact with the infectious agent[5]. However, not every exposure leads to an infection. Stress is one of many factors that can influence an individual’s susceptibility to infection.
In a 2017 review, Arturo Casadevall, a microbiologist and immunologist at the Johns Hopkins Bloomberg School of Public Health, and Liise-anne Pirofski, a physician-scientist at the Albert Einstein College of Medicine, described 11 factors that can influence an individual’s susceptibility to a microbe[6]. These factors are microbiome, inoculum, sex, temperature, environment, age, chance, history, immunity, nutrition, and genetics. Casadevall and Pirofski also acknowledged that more attributes of susceptibility will likely be identified in the future. They explained that these attributes “create an enormity of combinations that can in turn translate into different outcomes of host-microbe encounters”. In short, this means that each individual’s mix of contributing factors determines whether or not they develop an infection following exposure to a microbe. For example, in some individuals exposure to SARS-CoV-2 will develop into COVID-19, whereas in others, exposure to the virus leads to zero symptoms.
A functioning immune system is one of the factors listed by Casadevall and Pirofski that affects whether someone develops a disease or not. The immune system is defined by the U.S. National Cancer Institute as a “complex network of cells, tissues, organs, and the substances they make that helps the body fight infections and other diseases”. How well a person’s immune system functions is determined by both genetics and nonheritable factors, including sleep, nutrition, exercise, and stress. Again, Barrett is correct that stress can impact immunity; however, stress is just one factor that determines how well someone’s immune system functions.
Barrett is right that stress can influence a person’s immune system thereby impacting an individual’s susceptibility to an infectious agent. But stress isn’t the only factor that influences a person’s susceptibility to a disease and, as we saw with COVID-19, even young and healthy adults can get seriously ill and even die after catching an infectious agent. Moreover, calling these factors a “cause” of the disease is imprecise and potentially misleading. An individual suffering chronic stress would not develop a cold without exposure to a virus that causes the common cold. As such, the virus remains the cause of infectious diseases.
REFERENCES
- 1 – Patel et al. (2020) Poverty, inequality and COVID-19: the forgotten vulnerable. Public Health.
- 2 – Cohen et al. (1998) Type of stressors that increase susceptibility to the common cold. Health Psychology.
- 3 – Jacobs et al. (2013) Human rhinoviruses. Clinical Microbiology Reviews.
- 4 – Segerstorm et al. (2004) Psychological stress and the human immune system: A meta-analytic study of 30 years of inquiry. Psychological Bulletin.
- 5 – Barreto et al. (2006). Infectious diseases epidemiology. Journal of Epidemiology and Community Health.
- 6 – Casadevell et al. (2017) What is a host? Attributes of Individual Susceptibility. Infection and Immunity.
UPDATE NOTE
Following publication of this review, Dr. Barrett, via email, explained that her claim reflected a holistic approach to disease, one that ‘acknowledge[s] that most biological systems emerge from a multitude of weak, interacting causes, not from a single, isolated, strong cause.’ Her goal was not to deny the causal importance of a virus for disease, but to highlight the importance of other factors that often play a role.