- Health
COVID-19 treatments can improve a patient’s survival and recovery, but don’t replace the individual and community benefits of vaccination
Key takeaway
Treatments are intended to reduce the severity of disease and accelerate the recovery of patients that are already sick. While they complement vaccines and other public health measures to reduce the threat posed by a disease, they don’t replace the benefits provided by vaccination. Unlike vaccines, treatments cannot prevent disease. Apart from protecting an individual from disease, vaccines help to reduce transmission, thereby protecting others around the vaccinated individual and benefiting the wider community.
Reviewed content
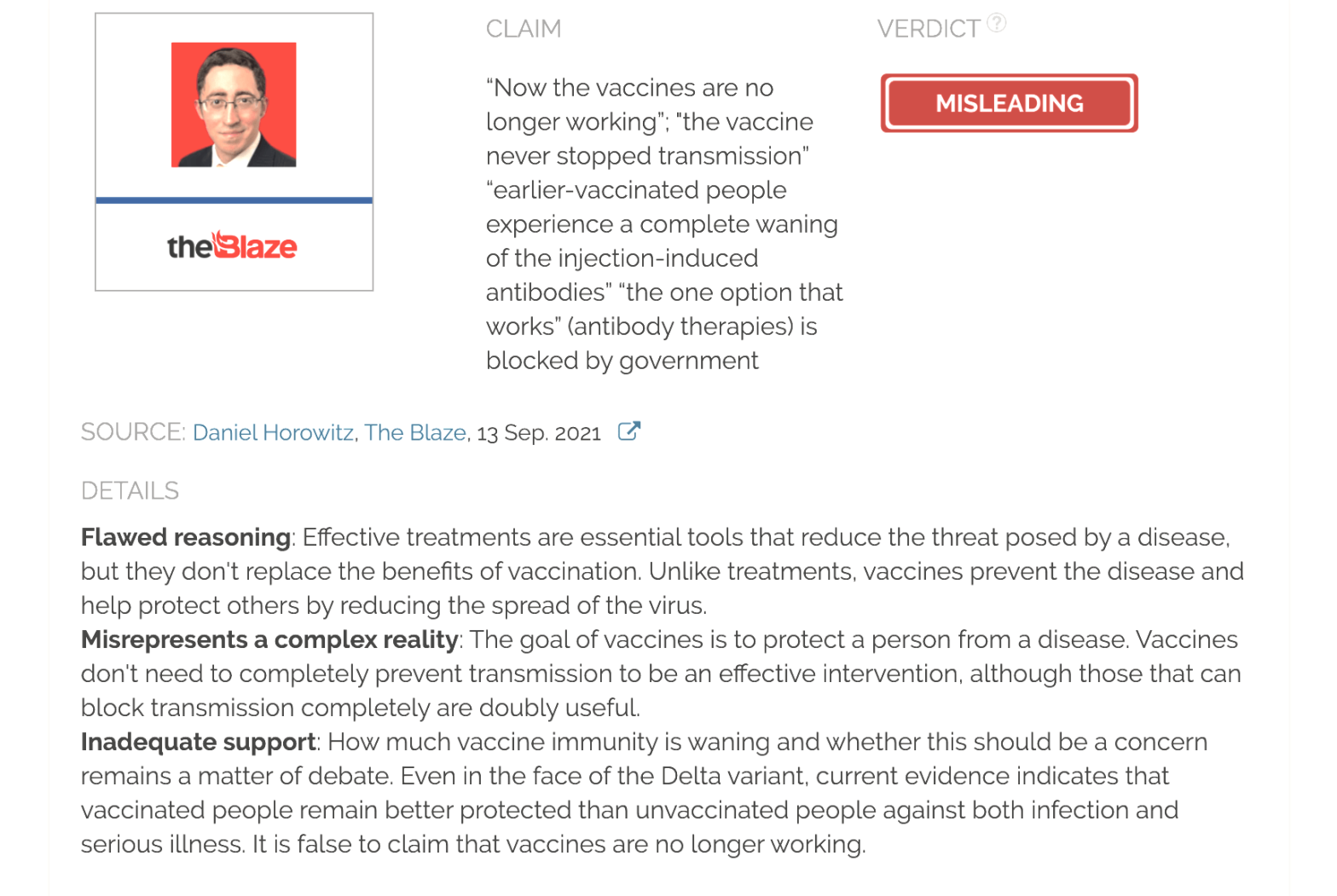
Verdict:
Claim:
“Now the vaccines are no longer working“; “the vaccine never stopped transmission“; “earlier-vaccinated people experience a complete waning of the injection-induced antibodies”; antibody therapy, “the one option that works”, is blocked by the government
Verdict detail
Flawed reasoning: Effective treatments are essential tools that reduce the threat posed by a disease, but they don't replace the benefits of vaccination. Unlike treatments, vaccines prevent the disease and help protect others by reducing the spread of the virus.
Misrepresents a complex reality: The goal of vaccines is to protect a person from a disease. Vaccines don't need to completely prevent transmission to be an effective intervention, although those that can block transmission completely are doubly useful.
Inadequate support: How much vaccine immunity is waning and whether this should be a concern remains a matter of debate. Even in the face of the Delta variant, current evidence indicates that vaccinated people remain better protected than unvaccinated people against both infection and serious illness. It is false to claim that vaccines are no longer working.
Full Claim
Now the vaccines are no longer working; “the vaccine never stopped transmission — indeed, the virus is spreading more than ever in highly vaccinated areas“; “every day this goes on, more of the earlier-vaccinated people experience a complete waning of the injection-induced antibodies”; “As vaccinated [COVID-19] hospitalizations soar, government blocks the one option that works [antibody therapies]”
Review
During the summer of 2021, many countries experienced a new COVID-19 surge mainly driven by the spread of the more contagious Delta variant. First identified in India in October 2020, this variant became rapidly dominant in many countries including the U.S., emerging as a game-changer in the pandemic.
Some interpreted this as evidence that vaccination is ineffective at protecting people against the disease. One example is this article published by The Blaze on 13 September 2021, claiming that “early treatments should replace useless vaccination strategies”. But this claim is rooted in a misunderstanding of the differences between what vaccines and treatments can achieve.
The main benefit of vaccines is to protect people from disease, without exposing them to the risk of disease. COVID-19 vaccines also reduce the risk of infection, which indirectly protects others from exposure by lowering the spread of the virus. In contrast, treatments aim to prevent disease progression or improve recovery in already infected individuals. This approach only protects the individual who receives the treatment and has more risks because it implies exposure to the disease.
The article suggested that COVID-19 vaccines are ineffective based on the arguments that vaccines “never stopped transmission” and earlier-vaccinated people are experiencing a “complete waning” of vaccine immunity. These claims are inaccurate and misleading in several ways, as we explain below.
Firstly, the main goal of vaccines is not to block all transmission but to prevent people from getting seriously ill or dying. While blocking infection and transmission to others makes a vaccine far more effective at curbing the spread of infectious diseases, it isn’t required for the vaccine to be effective. All approved and authorized COVID-19 vaccines offer robust protection against severe illness and death, even from the Delta variant. Therefore, vaccination remains the best protection against the disease.
Secondly, our previous experience with other vaccines demonstrates that even vaccines that don’t fully block transmission can still effectively reduce the spread of infectious diseases. One example is the rotavirus vaccine. Although the vaccine is “only” 74% effective against symptomatic cases and about 40% against transmission[1], its introduction in the U.S. in 2006 reduced the number of cases by 90%. Despite not stopping transmission completely, vaccines were able to eliminate polio from the U.S. and decrease the prevalence of diseases like diphtheria, measles, mumps, and rubella by 99%[2].
By reducing the risk of infection and the severity of the disease, COVID-19 vaccines lower viral spread and transmission. Early data from several countries, including Israel and the U.S., showed that mRNA COVID-19 vaccines prevented about 90% of infections in real-world conditions[3,4]. As a result, the number of new COVID-19 cases, hospitalizations, and deaths dropped drastically, particularly in countries with higher vaccination rates, like Israel and the U.K.
With the spread of the Delta variant, several countries reported a reduction of vaccines’ effectiveness against infection. In late July 2021, the Israeli Health Ministry released preliminary data indicating that the Pfizer-BioNTech COVID-19 vaccine protection against infection had dropped from the initial 91% to just 39%. However, reports from the U.S. and the U.K. offered different figures, ranging from 60 to 80% effectiveness against the Delta variant[5-8].
In this context, the Blaze article cited the “imperfect vaccine hypothesis” to claim that “mass vaccination appears to have made the virus worse”. According to this hypothesis, vaccines that prevent disease but don’t block infection and transmission cause selection pressure towards more virulent variants. Emma Hodcroft, an epidemiologist at the University of Bern, told Health Feedback that “any type of immunity present in the population will provide a selection pressure for the virus”, regardless of whether it comes from vaccines or previous infection. However, no evidence indicates that COVID-19 vaccines are making the virus more dangerous, as Health Feedback explained in earlier reviews here, here, and here. In fact, such an effect has never been observed in humans, only in poultry vaccinated against Marek’s disease.
An August 2021 preprint from the University of Maryland that hasn’t undergone peer-review yet also contradicts this argument. The authors found that the mutation frequency of SARS-CoV-2 in 20 countries correlated inversely with vaccination coverage[9]. In other words, countries with higher vaccination rates observed fewer mutations than those with lower vaccination rates. These results are preliminary, but are in line with the hypothesis by scientists that, by reducing viral spread, vaccination prevents the emergence of new variants, contrary to the article’s claim.
More recently, Israel reported that people who were vaccinated in January 2021 were at a higher risk of getting infected than those who received the vaccine three months later[10]. In parallel, other studies reported a steady decline of antibody levels in vaccinated individuals[11,12]. These data raised concerns about waning vaccine immunity, particularly in the face of the Delta variant.
However, the authors of the Israeli study and other scientists warned that these preliminary analyses might contain inaccurate data and be prone to bias. For example, people vaccinated at the early stages of the vaccination campaign tend to be older and have higher-risk professions than those vaccinated at later stages. The adherence to other public health measures such as physical distancing or mask-wearing might also have changed over time or according to vaccination status. Also, antibodies are only one player in the immune system’s defense. Cellular immune responses involving B and T cells are longer lasting than antibodies and might be enough to protect the person against disease[13,14].
Therefore, the debate about whether the results cited above show waning vaccine immunity and if this should be a concern is still ongoing. Further studies are needed to assess the duration of vaccine immunity and whether the increase in breakthrough infections is due to waning immunity, other factors like the spread of the Delta variant and the relaxation of other public health measures, or a combination of both. Some scientists believe that the problem has been overstated because breakthrough infections continue to be rare. Furthermore, vaccine protection against severe disease and death remains robust[15].
Indeed, current evidence indicates that vaccinated people remain better protected than unvaccinated people, despite the Delta variant. In August 2021, two studies published in Morbidity and Mortality Weekly Report evaluated the number of COVID-19 cases, hospitalizations, and deaths by vaccination status in New York and Los Angeles county between May and July 2021[6,16]. Although new COVID-19 cases increased among both unvaccinated and fully vaccinated adults, both studies reported lower rates among fully vaccinated people.
In Los Angeles, unvaccinated and partially vaccinated people accounted for 75% of the infections in July 2021, when the Delta variant was already dominant. At this point, unvaccinated people were five times more likely to get infected and 29 times more likely to be hospitalized than fully vaccinated people. Along this line, the CDC COVID Data Tracker shows that those states with lower vaccination coverage are still the ones with higher rates of COVID-19 cases and deaths. These data demonstrate that the decline in COVID-19 vaccine effectiveness is far from the “complete waning” that the article claimed.
Finally, the Blaze article blamed the U.S. government for blocking “other promising therapeutic options”, briefly citing early treatment with hydroxychloroquine and ivermectin. But neither of these drugs has proven effective against COVID-19, and public health authorities recommend against their use outside of clinical trials.
The article also touted monoclonal antibody treatments. Antibody therapies appear to be very effective in preventing hospitalization and death when given early in infection, and several have already received Emergency Use Authorization by the U.S. Food and Drug Administration (FDA).
The treatment consists in infusing the patient with laboratory-produced antibodies similar to those produced naturally by the body in response to an infection. The antibodies recognize the spike protein of the virus and prevent its entry into the cells.
But as the New York Times pointed out, monoclonal antibody treatments alone cannot tackle the COVID-19 pandemic:
“Doctors have warned that antibody treatments alone cannot keep pace with ballooning outbreaks. Whereas any one vaccination protects untold others from exposure, a single infusion only helps a single patient. Infusions must be given within 10 days of symptoms; they are unhelpful to most hospitalized patients. And receiving the antibodies once does not keep people from becoming seriously ill if they catch the virus again later.”
Surprisingly, antibody treatments have become very popular among people opposing COVID-19 vaccines, despite being also recently developed and not yet fully approved by the FDA. This led to a great surge in demand in U.S. states with low vaccination rates, including Florida, Texas, Mississippi, Tennessee, and Alabama. Rather than “blocking” these therapies, as the article claimed, the U.S. federal government covers their cost (about $2,100 per dose) for people at high risk of progressing to severe COVID-19. However, the increase in demand prompted the U.S. government to limit supplies in September 2021 to avoid shortages.
In summary, the fact that COVID-19 vaccines are less effective at preventing infections caused by the Delta variant compared to previous variants doesn’t render them useless. COVID-19 vaccines remain highly effective at preventing serious illness and death. Vaccines also reduce the risk of infection, even those caused by the Delta variant, thus lowering viral transmission within the community.
While certain treatments, such as monoclonal antibody therapy, can be effective at reducing disease severity and improving recovery in some patients, they don’t carry the same benefits as vaccination. Such treatments can only be used in certain cases and don’t provide protection to others. The article’s framing of monoclonal antibody therapy and clinically unproven treatments like hydroxychloroquine as an alternative to COVID-19 vaccines is misleading and a false dichotomy. Both vaccines and effective treatments are important in the fight against COVID-19, and the availability of an effective treatment doesn’t render vaccines unnecessary.
REFERENCES
- 1 – Bennett et al. (2021) Community transmission of rotavirus infection in a vaccinated population in Blantyre, Malawi: a prospective household cohort study. The Lancet.
- 2 – Roush et al. (2007) Historical Comparisons of Morbidity and Mortality for Vaccine-Preventable Diseases in the United States. JAMA.
- 3 – Dagan et al. (2021) BNT162b2 mRNA Covid-19 Vaccine in a Nationwide Mass Vaccination Setting. New England Journal of Medicine.
- 4 – Thompson et al. (2021) Interim Estimates of Vaccine Effectiveness of BNT162b2 and mRNA-1273 COVID-19 Vaccines in Preventing SARS-CoV-2 Infection Among Health Care Personnel, First Responders, and Other Essential and Frontline Workers — Eight U.S. Locations, December 2020–March 2021. Morbidity and Mortality Weekly Report.
- 5 – Fowlkes et al. (2021) Effectiveness of COVID-19 Vaccines in Preventing SARS-CoV-2 Infection Among Frontline Workers Before and During B.1.617.2 (Delta) Variant Predominance — Eight U.S. Locations, December 2020–August 2021. Morbidity and Mortality Weekly Report.
- 6 – Rosenberg et al. (2021) New COVID-19 Cases and Hospitalizations Among Adults, by Vaccination Status — New York, May 3–July 25, 2021. Morbidity and Mortality Weekly Report.
- 7 – Puranik et al. (2021) Comparison of two highly-effective mRNA vaccines for COVID-19 during periods of Alpha and Delta variant prevalence. medRxiv. [Note: The study is a preprint that hasn’t yet been peer-reviewed.]
- 8 – Pouwels et al. (2021) Impact of Delta on viral burden and vaccine effectiveness against new SARS-CoV-2 infections in the UK. medRxiv. [Note: The study is a preprint that hasn’t yet been peer-reviewed.]
- 9 – Yeh et al. (2021) Full vaccination is imperative to suppress SARS-CoV-2 delta variant mutation frequency. medRxiv. [Note: The study is a preprint that hasn’t yet been peer-reviewed.]
- 10 – Goldberg et al. (2021) Waning immunity of the BNT162b2 vaccine: A nationwide study from Israel. medRxiv. [Note: The study is a preprint that hasn’t yet been peer-reviewed.]
- 11 – Gaebler et al. (2021) Evolution of antibody immunity to SARS-CoV-2. Nature.
- 12 – Naaber et al. (2021) Dynamics of antibody response to BNT162b2 vaccine after six months: a longitudinal prospective study. The Lancet Regional Health — Europe.
- 13 – Goel et al. (2021) mRNA Vaccination Induces Durable Immune Memory to SARS-CoV-2 with Continued Evolution to Variants of Concern. bioRxiv. [Note: The study is a preprint that hasn’t yet been peer-reviewed.]
- 14 – Dan et al. (2021) Immunological memory to SARS-CoV-2 assessed for up to 8 months after infection. Science.
- 15 – Tenforde et al. Sustained Effectiveness of Pfizer-BioNTech and Moderna Vaccines Against COVID-19 Associated Hospitalizations Among Adults — United States, March–July 2021. Morbidity and Mortality Weekly Report.
- 16 – Griffin et al. (2021) SARS-CoV-2 Infections and Hospitalizations Among Persons Aged ≥16 Years, by Vaccination Status — Los Angeles County, California, May 1–July 25, 2021. Morbidity and Mortality Weekly Report.