- Health
Claims that long COVID doesn’t exist misrepresent study by Queensland Health researchers
Key takeaway
A proportion of people who have COVID-19 experience lingering symptoms following acute infection. These symptoms include fatigue, brain fog, changes in smell and taste, and persistent pain. Collectively, these symptoms are known as long COVID. Other viral infections, like the flu, are also known to produce the same symptoms in a subset of people. Research on why long COVID happens to some and not others, and how the condition can be managed and treated, is ongoing.
Reviewed content
Verdict:
Claim:
Queensland Health Researchers find that long COVID doesn’t exist
Verdict detail
Misrepresents source: Neither the study nor Queensland’s public health agency claimed that long COVID doesn’t exist. On the contrary, the study found that a proportion of people with COVID-19 do experience long-term symptoms, only that these are similar to those experienced by people who had other viral infections. Queensland’s Chief Health Officer is on record stating that the long-term symptoms experienced by some COVID-19 patients are real.
Full Claim
“No such thing as ‘long COVID,’ health agency says in shocking claim: ‘Unnecessary fear’”; “Top government health chief declares 'long COVID' doesn't really exist, study finds flu impairs more people in the long term”; “Australia: Queensland Health Researchers Claim ‘Long COVID’ Isn’t Real, Calls It ‘Unnecessary Fear’”
Review
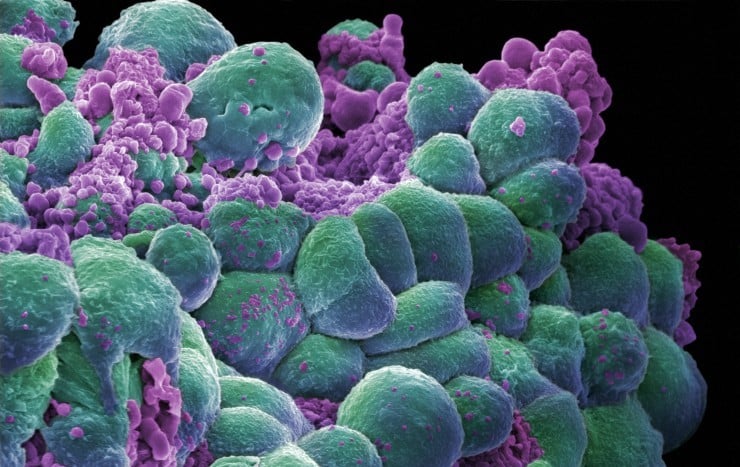
In March 2024, articles began circulating on social media platforms, alleging that Australian health officials claimed long COVID “isn’t real” or that it “doesn’t exist”. Examples of such articles appeared in the New York Post, The Blaze, and One American News Network. All three outlets have published misinformation about COVID-19 pandemic on multiple occasions (see here, here, and here).
The articles’ claims are purportedly based on the findings of a study co-authored by John Gerrard, Queensland’s Chief Health Officer.
The complete study has yet to be peer-reviewed or published, but its key findings were announced in a press release from the European Congress of Clinical Microbiology and Infectious Diseases. The press release stated that the findings would be presented at the congress, which will take place in Barcelona, Spain, at the end of April 2024.
The press release summed up the study’s conclusion as “Long COVID ‘indistinguishable’ from other post-viral syndromes a year after infection” and that it found “no evidence of worse post-viral symptoms or functional impairment a year after infection”.
In this review, we show why claims that the study found long COVID doesn’t exist grossly misrepresent the study and the position of Queensland’s Chief Health Officer.
What did the study do?
The study follows up on an earlier published study in the journal BMJ Public Health, also co-authored by Gerrard[1]. That earlier study surveyed roughly 3,100 adults three months after they were diagnosed with COVID-19 or flu by PCR testing.
The survey was conducted using a questionnaire delivered to participants via SMS. It asked participants whether they were still experiencing symptoms related to their COVID-19 or flu diagnosis, and if so, what impact these symptoms had on their daily life (functional impairment).
That earlier study found that adults with COVID-19 weren’t more likely to experience ongoing symptoms or to experience moderate to severe functional impairment than adults with a non-COVIDflu viral infection.
The follow-up study used the same method to survey people. This time, it surveyed a larger group (roughly 5,100 adults) one year after they developed symptoms of respiratory infection in 2022. This group had sought out a PCR test for COVID-19; those who tested negative for COVID-19 were also tested for influenza via PCR.
The researchers then compared ongoing symptoms and impairment between the group that tested positive for COVID-19 and the group that tested negative for COVID-19.
The researchers found that 16% of all respondents reported ongoing symptoms a year later, and 3.6% reported moderate-to-severe functional impairment in their activities of daily life. However, it found that those who tested positive for COVID-19 were just as likely as those who tested negative to have moderate to severe functional impairment.
This led the researchers to conclude that long COVID is a post-viral syndrome, like those that occur after infection with viruses that we’ve known about for a long time, such as the flu.
It’s important to note the study’s limitations. Firstly, the study couldn’t identify those who were hospitalized or had preexisting illnesses. Those hospitalized for COVID-19 or who had preexisting illness would have been most likely to experience the most severe symptoms. As such, the study may not have captured the full spectrum of long COVID.
Secondly, the study’s findings relate to a time when the Omicron variant was dominant. Some research suggests that the Omicron variant is associated with a lower risk of long COVID compared to other SARS-CoV-2 variants[2,3]. This means that the findings may not be representative of long COVID following infection by variants that aren’t Omicron, which were dominant in 2020 and 2021.
Thirdly, more than 90% of people in Queensland had been vaccinated in the period that the study examined. Since COVID-19 vaccination is associated with a lower risk of developing long COVID[4,5], the results may not be generalizable to a population that is largely unvaccinated.
The study showed that long-term effects of COVID-19 exist, but resemble those seen after other viral infections
The study’s findings that a proportion of people who had COVID-19 experience long-term symptoms like fatigue and brain fog—which can lead to significant limitations in daily life for some—show that COVID-19 can and does lead to long-term repercussions. Moreover, the long-term effects of COVID-19 are documented and described in multiple published studies[6-8].
Therefore, the study demonstrated the opposite of what headlines by the New York Post and The Blaze claim: long COVID exists and that it significantly affects people’s lives. What the researchers also found was that long COVID resembled post-viral syndrome that also develops in some people after other viral infections, like flu.
In fact, scientists have known about post-viral syndrome for decades, as infectious diseases researcher and professor Monica Gandhi wrote in this article for The Lancet:
“The public’s awareness of post-viral sequelae has been heightened by the COVID-19 pandemic, but infectious diseases experts have been aware of persisting symptoms following viral infections for more than a century. Post-influenza (an RNA virus) syndromes were first described following the 1918 influenza pandemic, including ‘encephalitis lethargica’, a relatively vague syndrome of ‘marked lethargy’ often accompanied by neurological symptoms. Post-viral syndromes have been described following Epstein-Barr virus, cytomegalovirus, herpes simplex virus (all DNA viruses), and measles (an RNA virus) infections, with chronic inflammation in the setting of elevated antibody titres to these viruses invoked as the pathophysiological mechanism.”
Science Feedback also reached out to Queensland Health for comment. In response, a representative of the media team directed us to the abstract for the study, an interview with Gerrard published by the Australian Broadcasting Corporation (ABC) on 14 March 2024, and a press conference he held on 15 March 2024.
The interview and the press conference clearly establish Queensland Health’s position on long-term COVID-19 effects.
In the ABC interview, Gerrard stated that “[p]ost-viral syndromes do occur. We’re absolutely saying that it does exist”. At the press conference on 15 March 2024, Gerrard reiterated this message, stating that “these symptoms and these long-term effects of COVID are real”.
Disagreement over call to stop using the term “long COVID”
What appears to be a point of contention is Gerrard’s call to stop using the term “long COVID”. He asserted that using the term long COVID “causes unnecessary fear. It implies that there is something particularly sinister and ominous about COVID-19”.
“Our evidence suggests that there isn’t, that it is not dissimilar to other viruses. That does not mean that you can’t get these persistent symptoms following COVID-19, but you’re no more likely to get it after COVID than with other respiratory viruses,” he said, adding that using the term makes people more hypervigilant to symptoms and impedes recovery.
Other scientists have disagreed with Gerrard’s conclusion. In her article for The Conversation, Deborah Lupton, a professor at the University of New South Wales’ Centre for Social Research in Health, wrote:
“Gerrard and his team’s findings cannot substantiate these assertions. Their survey only documented symptoms and impairment after respiratory infections. It didn’t ask people how fearful they were, or whether a term such as long COVID made them especially vigilant, for example.”
Jeremy Nicholson, a professor of medicine at Murdoch University, also pointed out another limitation:
“The study is observational, based on reported symptoms with no physiological or detailed functional follow-up data. Without laboratory pathophysiological assessment of individual patients, it is impossible to say that this is indistinguishable from flu-related or any other post-viral syndrome.”
Philip Britton, a pediatric infectious diseases researcher and a member of the Long COVID Australia Collaboration, commented that Gerrard and colleagues’ conclusion that we should stop using the term long COVID “is overstated and potentially unhelpful”. “Long COVID has been a global phenomenon, recognised by WHO,” he added.
Conclusion
An as-yet unpublished study found that people who had COVID-19 experienced long-term effects at a rate similar to those who had a non-COVID viral infection. The study’s authors concluded that this made long COVID “indistinguishable” from post-viral syndrome caused by other viruses like flu. Based on their results, they called for the term “long COVID” to be scrapped.
Other experts have disagreed with these conclusions as the study didn’t offer sufficient evidence to substantiate these assertions.
However, what isn’t in doubt is the fact that long-term repercussions of COVID-19 do exist and that these can significantly affect a person’s day-to-day life. And the study observed both effects. Claims by the New York Post and others that the study found long COVID doesn’t exist misrepresent its findings.
UPDATE (26 March 2024):
After our evaluation was published, the New York Post corrected its headline to remove the inaccurate claim (archive of the original article). See the archive of the corrected article.
REFERENCES
- 1 – Brown et al. (2023) Ongoing symptoms and functional impairment 12 weeks after testing positive for SARS-CoV-2 or influenza in Australia: an observational cohort study. BMJ Public Health.
- 2 – Hedberg and Nauclér. (2024) Post–COVID-19 Condition After SARS-CoV-2 Infections During the Omicron Surge vs the Delta, Alpha, and Wild Type Periods in Stockholm, Sweden. The Journal of Infectious Diseases.
- 3 – Thaweethai et al. (2023) Development of a Definition of Postacute Sequelae of SARS-CoV-2 Infection. JAMA.
- 4 – Català et al. (2024) The effectiveness of COVID-19 vaccines to prevent long COVID symptoms: staggered cohort study of data from the UK, Spain, and Estonia. The Lancet Respiratory Medicine.
- 5 – Lam et al. (2024) Persistence in risk and effect of COVID-19 vaccination on long-term health consequences after SARS-CoV-2 infection. Nature Communications.
- 6 – Nalbandian et al. (2021) Post-acute COVID-19 syndrome. Nature Medicine.
- 7 – Michelen et al. (2021) Characterising long COVID: a living systematic review. BMJ Public Health.
- 8 – Davis et al. (2023) Long COVID: major findings, mechanisms and recommendations. Nature Reviews Microbiology.