- Health
Claim that previously infected people don’t transmit COVID-19 is unsupported, originates from misinterpretation of CDC’s FOIA response
Key takeaway
Although infrequent, some people who recovered from a SARS-CoV-2 infection can get reinfected and potentially transmit the virus to others. COVID-19 vaccines remain highly effective at preventing severe illness and death and can also benefit those who were previously infected by enhancing their protective immunity.
Reviewed content
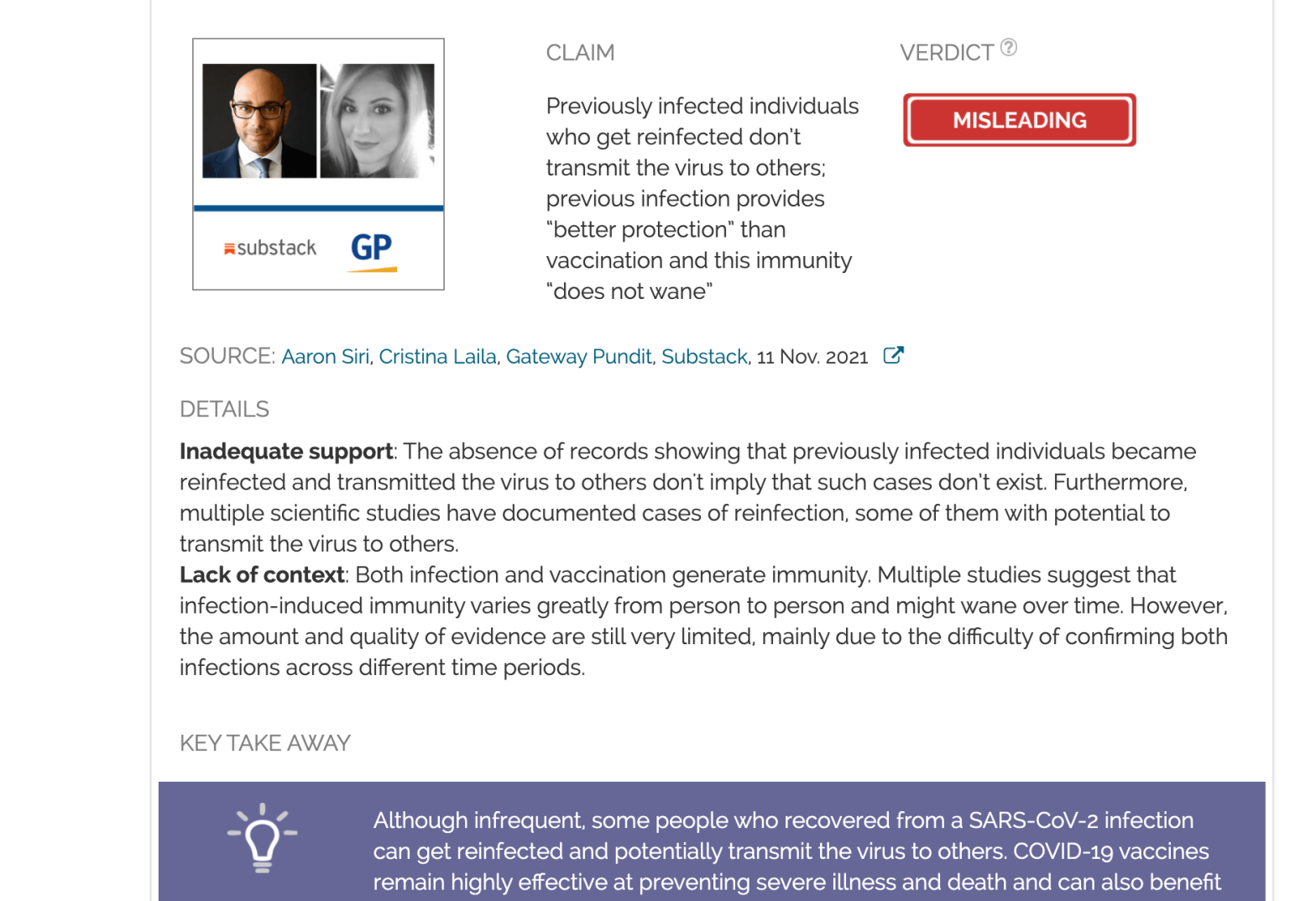
Verdict:
Claim:
Previously infected individuals who get reinfected don’t transmit the virus to others; previous infection provides “better protection” than vaccination and this immunity “does not wane”
Verdict detail
Inadequate support: The absence of records showing that previously infected individuals became reinfected and transmitted the virus to others don't imply that such cases don’t exist. Furthermore, multiple scientific studies have documented cases of reinfection, some of them with potential to transmit the virus to others.
Lack of context: Both infection and vaccination generate immunity. Multiple studies suggest that infection-induced immunity varies greatly from person to person and might wane over time. However, the amount and quality of evidence are still very limited, mainly due to the difficulty in confirming that a person was infected twice on different occasions.
Full Claim
“Every single peer reviewed study has found that the naturally immune have far greater than 99% protection from having COVID-19, and this immunity does not wane”; “while the vaccinated readily transmit the virus, not so for the naturally immune”; "A study examining T cell responses in Covid-19 convalescent individuals published earlier this year revealed natural immunity provides better protection against the China virus than vaccination."
Review
On 11 November 2021, Gateway Pundit published an article titled “CDC Admits It Has No Record of an Unvaccinated Person Spreading Covid After Recovering From Covid”. The article claimed that “natural immunity provides better protection against the China [COVID-19] virus than vaccination”, suggesting that vaccination is unnecessary for previously infected individuals.
These claims originated from a Freedom of Information Act (FOIA) request that the law firm Siri & Glimstad filed on 2 September 2021 on behalf of the Informed Consent Action Network (ICAN), an organization that opposes vaccines. In it, the firm requested from the U.S. Centers for Disease Control and Prevention (CDC) “documents reflecting any documented case of an individual who: (1) never received a COVID-19 vaccine; (2) was infected with COVID-19 once, recovered, and then later became infected again; and (3) transmitted SARS-CoV-2 to another person when reinfected.”
Aaron Siri, managing partner of Siri & Glimstad, published an article on Substack including the request and the response from the CDC, dated 5 November 2021:
”A search of our records failed to reveal any documents pertaining to your request. The CDC Emergency Operations Center (EOC) conveyed that this information is not collected”.
Based on the CDC’s response and a list of purportedly peer-reviewed studies cited in a letter to the CDC, the Substack article claimed that “while the vaccinated readily transmit the virus, not so for the naturally immune”. It also claimed that people who are “naturally immune have far greater than 99% protection from having COVID-19, and this immunity does not wane”.
Besides Gateway Pundit, multiple websites, including The Federalist, The Epoch Times, and The Defender promoted the claims in the Substack article, which received more than 50,000 interactions and 8,000 shares, according to the social media analytics tool CrowdTangle. The article’s claims also spread on social media platforms in the form of videos, memes, and posts (see examples here, here, here, and here).
However, absence of evidence isn’t evidence of absence. As we will explain below, cases of reinfection exist, and there is no scientific reason to assume that such cases aren’t infectious. In addition, many of the articles and posts support that infection-induced immunity is superior to vaccine-induced immunity by misrepresenting the results from scientific studies.
Absence of documented cases by the CDC of reinfected individuals transmitting the virus doesn’t mean these cases don’t exist
The Substack article presented the lack of CDC records as evidence that individuals who recovered from a SARS-CoV-2 infection don’t transmit the virus to others. Another website, Children’s Health Defense, cited Siri’s Substack article to support its claim that previously infected individuals may not need to get the COVID-19 vaccine. [Editor’s note: This paragraph was corrected; see here for details.]
It’s not the first time that ICAN resorted to FOIA requests in attempts to cast doubt over vaccine safety and effectiveness. In March 2020, ICAN suggested a link between vaccines and autism, ignoring a wide body of evidence that shows no association between both. Health Feedback reviewed that claim and found it to be inaccurate. Later in August 2020, ICAN misleadingly implied that there is no scientific evidence that aluminum adjuvants in vaccines are safe.
Multiple studies showed that patients who recovered from COVID-19 have a much lower risk of infection in the future, as opposed to non-infected individuals. However, as with vaccine-induced immunity, a previous infection doesn’t provide 100% protection, and cases of reinfection do occur, even though they are uncommon[1-6].
People who recover from a SARS-CoV-2 infection and become reinfected tend to have a lower viral load during the second infection than non-infected individuals. However, some of them might still carry a sufficient amount of virus to transmit it to others. One study published in The Lancet Respiratory Medicine evaluated virus shedding in 19 reinfected young, healthy individuals and found that four (25%) of them shed viable virus, meaning that the virus had infective potential. Furthermore, three of these individuals were asymptomatic, meaning they could potentially transmit the virus to others without knowing it[7].
But evidence about transmission by reinfected individuals is still preliminary and very limited, as public health authorities like Public Health England and the European Center for Disease Prevention and Control acknowledge. One main reason for this is that confirming reinfection isn’t always easy. For example, the CDC’s gold-standard confirmation for reinfection requires a positive PCR test confirming both primary infection and reinfection across two different periods. In addition, it requires analyzing the viral genomes of the viruses that caused both infections to confirm that it is indeed a case of reinfection rather than a persistent infection[8]. Other information, including a positive serological test, clinical symptoms compatible with COVID-19, or contact with a confirmed case could support a suspected reinfection but not confirm it definitely.
Because of these difficulties and the lack of a standard definition of what constitutes SARS-CoV-2 reinfection, different studies used a variety of criteria and testing methods to evaluate reinfections. The result is that it is difficult to compare one study to another and arrive at a consensus regarding the protection conferred by previous infection.
Study analyzing T cell responses included convalescent patients but not vaccinated individuals; claim that infection provides stronger immunity than vaccination based on this study is incorrect
Scientific evidence shows that both SARS-CoV-2 infection and COVID-19 vaccination create an immunological memory that enables the body to respond more rapidly and effectively if it encounters the virus in the future[9]. This response involves neutralizing antibodies—those that interfere with the ability of the virus to infect the cell—as well as B and T cells[10].
The article in Gateway Pundit claimed that one study evaluating T cell responses in COVID-19 convalescent individuals “revealed natural immunity provides better protection against the China virus than vaccination”. This claim misrepresents both the objective and the conclusions of the cited study, which is a brief report published in Open Forum Infectious Diseases[11].
The objective of this study was to evaluate whether T-cells from previously infected individuals recognized other SARS-CoV-2 variants. While the study did analyze the T-cell responses in 30 COVID-19 convalescent individuals, it didn’t include individuals who received the COVID-19 vaccine. Therefore, the results from the study don’t allow us to compare the T-cell response induced by infection with that induced by vaccination.
In fact, the authors highlighted:
“The data on CD8+ T-cell responses from these 30 convalescent individuals are also in line with another recent report showing that the great majority of CD4+ and CD8+ T-cell epitopes from the spike protein of the SARS-CoV-2 variants are also conserved in vaccinated individuals.”
Previous SARS-CoV-2 infection confers a certain degree of immunity but the level of protection it provides to different individuals appears less consistent than that from vaccination
The Substack article claimed that previous SARS-CoV-2 infection confers “greater than 99% protection from having COVID-19”. However, this figure exaggerates the protection provided by previous infection. Different studies reported reductions in the risk of reinfection for previously infected individuals ranging from 80% to 93%[2,4,12-14].
However, SARS-CoV-2 infection can involve different variants, viral levels, and clinical outcomes in different people, resulting in a variable level of protection against reinfection.
For example, one study conducted in Denmark before the spread of the Delta variant found that previous infection in people aged 65 years and older only reduced the risk of reinfection by 47.1% compared to around 80% in the overall population[4]. This suggests that the elderly don’t develop as much protection from previous infection compared to younger populations.
High levels of neutralizing antibodies appear to be the best current indicator of protection[14]. Several studies showed that the antibody levels that a person develops after infection highly depend on the severity of the disease. For example, one study that analyzed more than 3,500 households in China found that only 36% of the individuals who had an asymptomatic infection developed detectable levels of antibodies[15]. Another study conducted in Singapore and published in The Lancet Microbe also found that antibody levels in asymptomatic individuals and those with mild disease were lower and decreased more rapidly than in COVID-19 patients with severe disease[16].
All the above evidence indicates that a proportion of the people who recover from SARS-CoV-2 infection may remain susceptible to reinfection in the short term. In contrast, several studies suggest that full vaccination leads to a more consistent immune response[17-20].
Grant McFadden, director of the Biodesign Center for Immunotherapy, Vaccines and Virotherapy at Arizona State University, told USA Today: “Recovery from COVID results in very variable immunity to a second infection, and this is reflected in the wide range of anti-spike antibodies in recovered patients. On the other hand, the immunity from the vaccines (especially the messenger RNA versions) is much more uniform, both in terms of protection from COVID and in anti-spike antibody levels.”
Data about the duration of infection-induced immunity is still limited, but reinfections are likely to become more frequent over time
Data are still insufficient to draw conclusions on the long-term duration of protection against SARS-CoV-2 reinfection. Therefore, the Substack article’s claim that infection-induced immunity “does not wane” is currently unsupported.
There is evidence that antibody levels start declining within the first months after SARS-CoV-2 infection[21,22]. Some studies showed that at least 5% of infected people lose or don’t develop detectable levels of neutralizing antibodies within six months[23].
The study from Singapore found that the antibody levels developed after infection varied greatly among different patients, and so did the rate of antibody waning[16]. Among the 164 individuals included in the study, 63% (107) developed high levels of neutralizing antibodies with no or low waning over time. However, 27% (44) of the patients who developed an antibody response returned to undetectable antibody levels within the six-month follow-up of the study. In addition, 12% (19) of the individuals didn’t develop detectable antibody levels after the infection.
Multiple studies show that neutralizing antibodies developed after infection with other coronaviruses closely related to SARS-CoV-2 do wane in the long term[24-26]. Based on this previous evidence from other coronaviruses, U.S. researchers estimated the probability of SARS-CoV-2 reinfection over time[27]. The study, published in The Lancet Microbe in October 2021, estimated that reinfection with SARS-CoV-2 could likely occur within an average of 16 months after the first infection.
While there is limited data for making accurate estimates about the duration of infection-induced immunity, what we know from studies on other coronaviruses as well as studies about antibody levels after SARS-CoV-2 infection suggests that immunity is likely to wane over the long run, making reinfection more likely over time. For this reason, experts highlight the importance of practicing multiple protective measures, including vaccination, to minimize the risk.
Previous infection and vaccination aren’t mutually exclusive; instead, they complement each other to enhance protection
Determining how well previous infection and vaccination protect against COVID-19 is essential for public health decision-making. However, arguing that one type of immunity is better than the other is misleading and establishes a false dichotomy. False dichotomy, also called false dilemma, incorrectly presents a situation as only having two choices, when there are in fact more.
As Health Feedback explained in this Insight article, infection-induced immunity and vaccine-induced immunity aren’t mutually exclusive. On the contrary, immunologic data show that previously infected individuals who are vaccinated have enhanced protection compared to infection alone and against variants of the virus[28-30].
Conclusion
Both vaccination and previous infection confer protection against subsequent infections, hospitalization, and death. But data showing how much infection-induced immunity protects against reinfection, the duration of that immunity, and transmission by reinfected individuals is largely based on a few studies with a small number of reinfections. As such, there is uncertainty over how long infection-induced immunity lasts and whether reinfected people transmit.
Although a previously infected person is generally less likely to become infected again than a non-infected individual, infection-induced immunity varies greatly from person to person, and a proportion of individuals who recover from a SARS-CoV-2 infection remain susceptible to reinfection within the first months. Given the uncertainty about how well protected an individual is after infection, public health authorities like the U.S. Centers for Disease Control and Prevention (CDC) recommend that previously infected people also get vaccinated to reduce the risks as much as possible.
CORRECTION (31 Jan. 2022):
The review initially attributed the claim that previously infected people don’t need to get the COVID-19 vaccine to Siri’s Substack article. This is inaccurate; the review should have attributed that claim to another article by Children’s Health Defense that cited Siri’s Substack article as evidence for that claim. We have now corrected this error and lightly edited the review for clarity.
REFERENCES
- 1 – Lumley et al. (2021) Antibody Status and Incidence of SARS-CoV-2 Infection in Health Care Workers. New England Journal of Medicine.
- 2 – Hall et al. (2021) SARS-CoV-2 infection rates of antibody-positive compared with antibody-negative health-care workers in England: a large, multicentre, prospective cohort study (SIREN). The Lancet.
- 3 – Harvey et al. (2021) Association of SARS-CoV-2 Seropositive Antibody Test With Risk of Future Infection. JAMA International Medicine.
- 4 – Hansen et al. (2021) Assessment of protection against reinfection with SARS-CoV-2 among 4 million PCR-tested individuals in Denmark in 2020: a population-level observational study. The Lancet.
- 5 – Abu-Raddad et al. (2021) Assessment of the Risk of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Reinfection in an Intense Reexposure Setting. Clinical Infectious Diseases
- 6 – Tomassini et al. (2020) Setting the criteria for SARS-CoV-2 reinfection – six possible cases. Journal of Infection.
- 7 – Letizia et al. (2021) Viable virus shedding during SARS-CoV-2 reinfection. The Lancet Respiratory Medicine.
- 8 – To et al. (2020) Coronavirus Disease 2019 (COVID-19) Re-infection by a Phylogenetically Distinct Severe Acute Respiratory Syndrome Coronavirus 2 Strain Confirmed by Whole Genome Sequencing. Clinical Infectious Diseases.
- 9 – Pouwels et al. (2021) Effect of Delta variant on viral burden and vaccine effectiveness against new SARS-CoV-2 infections in the UK. Nature Medicine.
- 10 – Dan et al. (2021) Immunological memory to SARS-CoV-2 assessed for up to 8 months after infection. Science.
- 11 – Redd et al. (2021) CD8+ T-Cell Responses in COVID-19 Convalescent Individuals Target Conserved Epitopes From Multiple Prominent SARS-CoV-2 Circulating Variants. Open Forum Infectious Diseases.
- 12 – Sheehan et al. (2021) Reinfection Rates Among Patients Who Previously Tested Positive for Coronavirus Disease 2019: A Retrospective Cohort Study. Clinical Infectious Diseases.
- 13 – Vitale et al. (2021) Assessment of SARS-CoV-2 Reinfection 1 Year After Primary Infection in a Population in Lombardy, Italy. JAMA International Medicine.
- 14 – Addetia et al. (2020) Neutralizing Antibodies Correlate with Protection from SARS-CoV-2 in Humans during a Fishery Vessel Outbreak with a High Attack Rate. Journal of Clinical Microbiology.
- 15 – He et al. (2021) Seroprevalence and humoral immune durability of anti-SARS-CoV-2 antibodies in Wuhan, China: a longitudinal, population-level, cross-sectional study. The Lancet.
- 16 – Chia et al. (2021) Dynamics of SARS-CoV-2 neutralising antibody responses and duration of immunity: a longitudinal study. The Lancet Microbe.
- 17 – Jackson et al. (2020) An mRNA Vaccine against SARS-CoV-2 — Preliminary Report. New England Journal of Medicine.
- 18 – Walsh et al. (2020) Safety and Immunogenicity of Two RNA-Based Covid-19 Vaccine Candidates. New England Journal of Medicine.
- 19 – Lombardi et al. (2021) Mini Review Immunological Consequences of Immunization With COVID-19 mRNA Vaccines: Preliminary Results. Frontiers in Immunology.
- 20 – Israel et al. (2021) Large-scale study of antibody titer decay following BNT162b2 mRNA vaccine or SARS-CoV-2 infection. medRxiv. [Note: This is a preprint that has not yet been peer-reviewed at the time of this review’s publication.]
- 21 – Long et al. (2020) Clinical and immunological assessment of asymptomatic SARS-CoV-2 infections. Nature Medicine.
- 22 – Robbiani et al. (2020) Convergent antibody responses to SARS-CoV-2 in convalescent individuals. Nature.
- 23 – Seow et al. (2020) Longitudinal observation and decline of neutralizing antibody responses in the three months following SARS-CoV-2 infection in humans. Nature Microbiology.
- 24 – Wu et al. (2007) Duration of Antibody Responses after Severe Acute Respiratory Syndrome. Emerging Infectious Diseases.
- 25 – Alshukairi et al. (2016) Antibody response and disease severity in healthcare worker MERS survivors. Emerging Infectious Diseases.
- 26 – Edridge et al. (2020) Seasonal coronavirus protective immunity is short-lasting. Nature Medicine.
- 27 – Townsend et al. (2021) The durability of immunity against reinfection by SARS-CoV-2: a comparative evolutionary study. The Lancet Microbe.
- 28 – Wang et al. (2021) Naturally enhanced neutralizing breadth against SARS-CoV-2 one year after infection. Nature.
- 29 – Gallais et al. (2021) Evolution of antibody responses up to 13 months after SARS-CoV-2 infection and risk of reinfection. EBio Medicine.
- 30 – Stamatatos et al. (2021) mRNA vaccination boosts cross-variant neutralizing antibodies elicited by SARS-CoV-2 infection. Science.