- Health
Article by cardiologist Aseem Malhotra made unsupported claims about the benefits and risks of COVID-19 vaccination
Key takeaway
Scientific evidence from clinical trials and safety monitoring indicate that the COVID-19 vaccines are safe and effective. While severe reactions to the vaccine can occur, they are rare, and the most common side effects of vaccination are mild and go away within a few days. All available evidence indicates that being vaccinated is safer than not being vaccinated.
Reviewed content
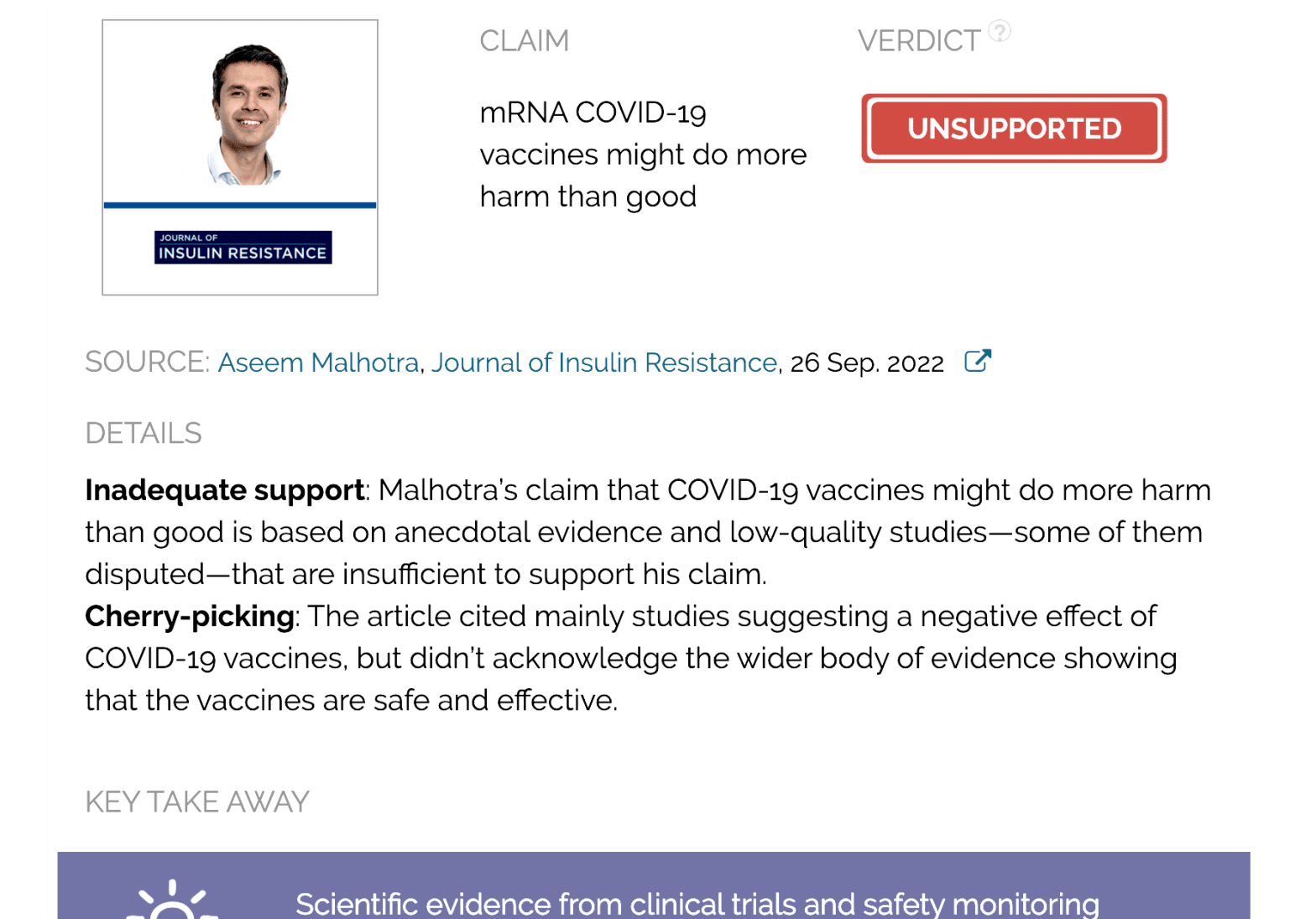
Verdict:
Claim:
mRNA COVID-19 vaccines might do more harm than good
Verdict detail
Inadequate support: Malhotra’s claim that COVID-19 vaccines might do more harm than good is based on anecdotal evidence and low-quality studies—some of them disputed—that are insufficient to support his claim.
Cherry-picking: The article cited mainly studies suggesting a negative effect of COVID-19 vaccines, but didn’t acknowledge the wider body of evidence showing that the vaccines are safe and effective.
Full Claim
Non-elderly population have “a greater risk of serious adverse events from the vaccines than being hospitalised from COVID-19”; safety data “are deeply concerning, especially in relation to cardiovascular safety”
Review
On 26 September 2022, cardiologist Aseem Malhotra published a two-part article (archived here and here) in the Journal of Insulin Resistance—of which Malhotra is an editor— calling for a global pause of mRNA vaccines. Part 1 of the article claimed to provide evidence that the likelihood of serious adverse events in the non-elderly population might be higher than the benefits of vaccination. The article defined the risks as “deeply concerning, especially in relation to cardiovascular safety”.
Malhotra repeated these claims in a 27 September 2022 press conference hosted by the World Council for Health, an organization that falsely linked COVID-19 vaccines to thousands of deaths and multiple alleged safety issues. Other speakers were scientist Tess Lawrie, co-founder of the organization, and pathologist Ryan Cole, who also spread misinformation about the safety of COVID-19 vaccines in the past.
In the article’s Acknowledgements section, Malhotra mentioned that Clare Craig and Alex Starling, members of the group Health Advisory and Recovery Team (HART), rendered assistance to him in the writing of the article. According to an investigation by Logically, this organization lobbied to promote COVID-19 misinformation and has links to conspiracy groups. In the press conference (timestamp 37:55), Malhotra confirmed the HART group’s involvement in the article.
Malhotra’s article received more than 14,000 interactions on Facebook and Twitter, according to the social media analytics tool CrowdTangle. But his claims circulated more widely on social media (see examples here and here), as they were picked up by Children’s Health Defense, an organization opposing vaccination, and outlets such as The Epoch Times and Washington Times, labeled as Questionable Sources by Media Bias Fact Check. Individuals who previously published misinformation about COVID-19 vaccines, like scientist Robert Malone and tech entrepreneur Steve Kirsch, also echoed the article.
As we will explain in this review, Malhotra’s analysis of the benefits and harms of the COVID-19 vaccines is misleading and based on cherry-picked evidence. Below, we will analyze in detail the most relevant pieces of evidence that Malhotra provided and explain why they are insufficient to support his claims.
Reanalysis of clinical trial data from Pfizer and Moderna
One of the main pieces of evidence in the article is a study published by Fraiman et al. in the journal Vaccine[1]. In it, the authors analyzed data from a previous study of adverse events reported in the clinical trials of the Pfizer-BioNTech and Moderna mRNA COVID-19 vaccines[2,3]. They concluded that “The excess risk of serious adverse events of special interest was higher than the risk reduction for COVID-19 hospitalization relative to the placebo group” in both Pfizer and Moderna trials.
To arrive at this conclusion, the authors calculated how many more serious adverse events occurred in the vaccinated group compared to the control group. They then compared this figure with the number of people hospitalized with COVID-19 during the clinical trials.
To determine what kind of adverse events would be considered as serious for the purposes of the study, the authors looked to the Priority List of COVID-19 Adverse events of special interest by the Brighton Collaboration (BC), a program of the nonprofit organization The Task Force for Global Health. This list includes adverse events that have been seen with COVID-19, as well as those with a proven or theoretical association with vaccines in general or with specific vaccine platforms.
The now-published study was initially available as a preprint—a manuscript that hasn’t undergone peer review—in June 2022. Health Feedback previously reviewed it and found that the authors’ analysis didn’t support their conclusion. Scientists such as surgeon and cancer researcher David Gorski, biostatistician Jeffrey S. Morris, and nanomedicine expert Susan Oliver pointed out several issues in the study that indicated potential p-hacking.
P-hacking (also known as data dredging or data snooping) is the manipulation of data analysis to make the results look statistically significant when they aren’t. The study by Fraiman et al. showed several signs suggesting that the authors had analyzed data in a manner that favored their hypothesis.
First, the Brighton document lists “adverse events of special interest” (AESI) mainly as specific clinical diagnoses, such as enteritis/colitis, arthritis, and encephalitis. In order for the authors to count the number of serious AESIs associated with COVID-19 vaccines, they needed to determine which serious adverse events (SAEs) recorded in the vaccines’ clinical trials corresponded to the AESIs listed in the Brighton document.
The decision of whether an SAE corresponded to a Brighton AESI rested on the opinion of two independent clinicians, and a third one if the first two disagreed without arriving at a consensus.
However, the reasons for considering certain SAEs as corresponding to the AESI list are unclear and inconsistent. For example, one Brighton AESI is enteritis/colitis, for which the corresponding adverse events would be diarrhea and vomiting. However, the authors included diarrhea but not vomiting when counting relevant SAEs. Another example is the authors’ inclusion of arthritis as a serious adverse event, but not osteoarthritis (a form of arthritis).
The authors also excluded “events related to COVID-19”. While this exclusion could make sense when focusing on potential side effects of the COVID-19 vaccines, it introduces an important bias by eliminating adverse events that are expected to be much more common in the control group than in the vaccinated group. This means that the study was less able to detect harms from COVID-19. Overall, these observations suggest that the adverse events that the authors chose to analyze were the result of cherry-picking.
Second, the authors compared the people hospitalized with COVID-19 with the total number of adverse events in the control and the vaccinated groups rather than the number of individuals who reported the adverse events. Since one person can suffer multiple adverse events but only one hospitalization, this analysis leads to an overcounting of adverse events and over-represents the harmful effects of vaccination compared to the risks of COVID-19. For example, a person who reported colitis, diarrhea, and abdominal pain, would be counted as three adverse events, even though the three occurred in the same person and are likely related.
Finally, some of the included adverse events, such as diarrhea, abdominal pain, and rash, aren’t equivalent to a COVID-19 hospitalization in terms of disease severity. This analysis also doesn’t take into account the benefits of vaccination in preventing COVID-19 complications other than hospitalization, including cardiovascular problems.
Given the methodological flaws in the study, the analysis is unreliable and doesn’t support the claim that vaccines cause more serious adverse events than the benefits they provide.
The efficacy of COVID-19 vaccines
Malhotra’s article referred to the absolute risk reduction (ARR) of 0.84% reported in Pfizer’s trial as “the true value of any treatment”, as compared to the reported relative risk reduction (RRR) of 95%. This comparison gives the impression that COVID-19 vaccines are ineffective or less effective than reported, which is incorrect and has been previously misused to downplay the benefit of COVID-19 vaccines.
The RRR and the ARR are two different and complementary ways of measuring the effect of vaccination. The RRR measures the risk of an event—for example, infection—in the treatment (vaccinated) group expressed as a proportion of the event rate in the control (unvaccinated) group. The ARR results from subtracting the event rate in the treatment group from that in the control group and represents the overall benefit of vaccination in the population.
While the ARR will always appear low compared to the RRR, this doesn’t mean that COVID-19 vaccines are ineffective, as Health Feedback explained earlier. In a Reuters fact-check, Natalie E. Dean, a biostatistician and assistant professor at Emory University, explained that the RRR is a “more meaningful” way than ARR to express how much a vaccine reduces the risk of COVID-19 because it is “irrespective of the transmission setting”.
In contrast, the ARR varies considerably depending on the transmission rate. An ARR of 0.84% in clinical trials simply indicates that the infection rate during the trial was low. This was due to the limited duration of the clinical trials and the strict COVID-19 control measures at that time, which translated into comparatively fewer infections.
However, the ARR increases when the number of infections rises, for example during the Delta and Omicron waves, because the vaccines’ benefits, specifically their ability to prevent COVID-19, becomes more apparent during infection waves[4].
Research shows that, contrary to what Malhotra suggested, COVID-19 vaccines do reduce the risk of infection and are highly effective against severe COVID-19 and death for everyone[5-7].
Serious adverse events following COVID-19 vaccination
Like any medical intervention, COVID-19 vaccines can cause side effects. The most common side effects of COVID-19 vaccines are mild and last only a few days. In contrast, severe reactions after COVID-19 vaccination are infrequent.
In the article, Malhotra suggested that COVID-19 vaccines are unsafe based on the “unprecedented” number of adverse event reports following COVID-19 vaccination compared to previous years and other vaccines. For that, he used data from the U.K. Yellow Card Scheme and the U.S. Vaccine Adverse Event Report System (VAERS).
However, this is a misuse of adverse event reports, as Health Feedback explained in earlier reviews. While these reports can be a starting point for investigating potential side effects of the vaccine, the reports alone don’t demonstrate that the vaccine caused or contributed to an adverse event. Therefore, the number of adverse events recorded after vaccination doesn’t indicate that the vaccine caused them or that the vaccine is unsafe.
Furthermore, COVID-19 vaccines have been the subject of “the most intense safety monitoring in US history”, according to the U.S. Centers for Disease Control and Prevention (CDC). This fact alone could explain a higher rate of adverse event reporting for COVID-19 vaccines compared to other vaccines.
Malhotra suggested that COVID-19 vaccines were associated with an increased risk of cardiovascular problems by citing a conference abstract published in Circulation. This abstract purportedly showed a 25% increase in the risk of a coronary event within two to ten weeks after receiving an mRNA COVID-19 vaccine.
The American Heart Association, which publishes the journal, was later notified about “potential errors” in the abstract and issued an expression of concern stating that the results “may not be reliable.” Jeffrey Morris, director of the division of biostatistics at the University of Pennsylvania, told FactCheck.org that “the lack of details on the patient selection, analysis approach, and other details,” make it “impossible to evaluate.”
Malhotra also cited “the disturbing findings” of another study claiming to show an association of COVID-19 vaccines with a 25% increase in emergency calls for acute coronary syndrome and cardiac arrest among people aged 16 to 39 in Israel. This study wasn’t published in Nature, as Malhotra claimed, but in Scientific Reports, another peer-reviewed journal that is part of Nature Portfolio. The study was heavily criticized for having serious methodological flaws, as FactCheck.org explained, and is currently under investigation by the journal’s editors.
Risk of heart inflammation following COVID-19 vaccination is lower than that following COVID-19
Malhotra claimed that “one of the most common mRNA COVID-19 vaccine-induced harms is myocarditis”, an inflammation of the heart muscle. He added that cases of myocarditis “rocketed from spring 2021 when vaccines were rolled out to the younger cohorts” and although these cases are “not often fatal”, they might cause “likely permanent” heart muscle injury with potential negative effects in the long term. There is currently no scientific evidence supporting these claims.
It is true that mRNA COVID-19 vaccines have been associated with an increased risk of myocarditis, particularly among young males. But some have exaggerated this risk to promote the narrative that COVID-19 vaccines are unsafe, as Health Feedback documented in earlier reviews.
One of the most recent studies evaluating the risk of post-vaccine myocarditis was published in The Lancet in June 2022[8]. Using data from large U.S. healthcare databases, the study found an increased risk of myocarditis and pericarditis after receiving an mRNA vaccine, particularly in men aged 18–25 years and after a second dose. The rate of heart inflammation in this population after the second dose was 2.17 per 100,000 people who received the Pfizer-BioNTech vaccine, and 1.71 per 100,000 people who received the Moderna vaccine. The authors concluded that the benefits of vaccination continued to outweigh the risk of such rare cases of heart inflammation.
In fact, current evidence indicates that post-vaccine myocarditis is typically mild and self-resolves quickly[9]. This risk is also much lower than the risk of heart complications after getting COVID-19 itself, which can increase the risk of cardiovascular disease for up to one year[10].
A few studies did find that people who had post-vaccine myocarditis showed heart abnormalities for up to eight months after recovering[11-13]. But what Malhotra didn’t mention is that these abnormalities were generally less severe and caused fewer complications than typical myocarditis due to other causes. This, together with the good clinical outcomes of the patients, don’t suggest that post-vaccine myocarditis has long-term health implications, as Malhotra suggested. However, additional studies with longer follow-ups would provide us with much more information about the consequences of post-vaccine myocarditis.
Malhotra also claimed that no clinical trial data had demonstrated that vaccination reduces the risk of myocarditis in subsequent infection. He added that “in fact the risks may be additive”, without providing evidence for this claim. It’s important to keep in mind that clinical trials usually don’t have the capacity to detect very rare adverse events such as the cases of myocarditis associated with COVID-19 vaccination, which occur at a very low rate and might only become apparent in populations larger than those typically involved in trials.
But there is one study published in Circulation in August 2022 that does address Malhotra’s question about whether the vaccines reduce myocarditis risk following infection[14]. This study analyzed the risk of myocarditis after COVID-19 infection and after vaccination in records from England’s National Immunization database for more than 40 million people aged 13 and older.
The analysis showed that people infected with SARS-CoV-2 before receiving a vaccine were 11 times more at risk for developing myocarditis within 28 days of testing positive for the virus than people who didn’t test positive. The risk of developing myocarditis following infection halved in the people who had received at least one dose of a COVID-19 vaccine, suggesting that the vaccines do protect against post-COVID myocarditis.
Lower COVID-19 deaths and all-cause deaths in people who got vaccinated against COVID-19
Malhotra’s article stated that “The most objective determinant of whether the benefits of the vaccines outweigh the harms is by analyzing its effects on all-cause mortality”. He claimed that the results from clinical trials didn’t show a significant benefit in reducing “serious illness or COVID-19 mortality” over the six months of trial. Instead, he said, all-cause mortality was slightly higher in the vaccinated group (19 deaths) compared to the control group (17 deaths) during an additional follow-up period of around four months.
However, Malhotra misrepresented the conclusions of the clinical review memorandum by the U.S. Food and Drug Administration regarding all-cause mortality during Pfizer’s trial. Page 82 of this document, which Malhotra cited as a reference, clearly stated:
“Overall, deaths and SAEs were reported by similar proportions of participants in both treatment groups. A total of 38 deaths occurred in the reporting period (19 deaths in the BNT162b2 group, 17 in placebo and 2 in the placebo/BNT162b2 group). More deaths occurred in the older age group, as expected due to increased age and comorbidities. All deaths represent events that occur in the general population of the age groups where they occurred, at a similar rate. The frequency of non-fatal serious adverse events was low without meaningful imbalances between treatment groups.” [emphasis added]
As we explained above, the original trials observed a limited number of infections that made it difficult for researchers to accurately estimate the reduction in COVID-19 mortality. However, since then, several studies have used real-world data and showed that mRNA COVID-19 vaccines are highly effective at preventing severe disease and COVID-19 death[15-20].
In fact, recent research found that COVID-19 vaccines weren’t associated with an increased risk of mortality but instead with a lower all-cause mortality. The U.S. CDC evaluated all-cause mortality among 6.4 million vaccinated and 4.6 million unvaccinated persons and found that people who received any of the three COVID-19 vaccines authorized in the U.S. were up to three times less likely to die from any cause than those who didn’t receive a vaccine[21]. This finding is inconsistent with the claim that vaccinated people are more likely to die compared to unvaccinated people.
Malhotra’s article provides insufficient evidence for informing public health decisions
Malhotra and those promoting his claims presented the article in the Journal of Insulin Resistance as a peer-reviewed scientific study offering “real evidence-based medicine” as opposed to that guiding public health policies. As we explained above, that isn’t the case.
Literature reviews come in many forms, but not all are equally reliable. The practice of evidence-based medicine uses a specific methodology called systematic review. This type of review aims to answer a research question by identifying all the studies that meet a pre-specified eligibility criteria. The eligibility criteria also involves assessing the quality of the studies evaluated[22]. This approach makes systematic reviews reproducible and minimizes the risk of bias.
This methodology contrasts with that exhibited in Malhotra’s article, which used low-quality evidence—including disputed studies, anecdotes, and anonymous sources—all of which tended to support Malhotra’s hypotheses, but failed to also consider peer-reviewed published studies that contradict Malhotra’s hypotheses, suggesting that the conclusions are affected by bias.
In summary, the aforementioned limitations make Malhotra’s article unreliable for informing public health decisions about COVID-19 vaccination campaigns. The article cherry-picked evidence supporting the narrative that COVID-19 vaccines are ineffective and possibly harmful, while ignoring the larger body of evidence showing that COVID-19 vaccines are safe and effective.
READ MORE
In Part 2 of the article, Malhotra again used cherry-picked information to accuse social media platforms, doctors, scientists, and medical authorities of spreading misinformation about COVID-19 vaccines. David Gorski debunked it in this blog post for Science-Based Medicine.
REFERENCES
- 1 – Fraiman et al. (2022) Serious adverse events of special interest following mRNA COVID-19 vaccination in randomized trials in adults. Vaccine.
- 2 – Polack et al. (2020) Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine. The New England Journal of Medicine.
- 3 – Baden et al. (2021) Efficacy and Safety of the mRNA-1273 SARS-CoV-2 Vaccine. The New England Journal of Medicine.
- 4 – Marabotti (2021) Efficacy and effectiveness of covid-19 vaccine – absolute vs. relative risk reduction. Expert Review of Vaccines.
- 5 – Rennert et al. (2022) Effectiveness and protection duration of Covid-19 vaccines and previous infection against any SARS-CoV-2 infection in young adults. Nature Communications.
- 6 – Fowlkes et al. (2022) Effectiveness of 2-Dose BNT162b2 (Pfizer BioNTech) mRNA Vaccine in Preventing SARS-CoV-2 Infection Among Children Aged 5–11 Years and Adolescents Aged 12–15 Years — PROTECT Cohort, July 2021–February 2022. Morbidity and Mortality Weekly Report.
- 7 – Lin et al. (2022) Effects of Vaccination and Previous Infection on Omicron Infections in Children. The New England Journal of Medicine.
- 8 – Wong et al. (2022) Risk of myocarditis and pericarditis after the COVID-19 mRNA vaccination in the USA: a cohort study in claims databases. Lancet.
- 9 – Oster et al. (2022) Myocarditis Cases Reported After mRNA-Based COVID-19 Vaccination in the US From December 2020 to August 2021. JAMA.
- 10 – Xie et al. (2022) Long-term cardiovascular outcomes of COVID-19. Nature Medicine.
- 11 – Hadley et al. (2022) Follow-up cardiac magnetic resonance in children with vaccine-associated myocarditis. European Journal of Pediatrics.
- 12 – Fronza et al. (2022) Myocardial Injury Pattern at MRI in COVID-19 Vaccine–Associated Myocarditis. Radiology
- 13 – Schauer et al. (2022) Persistent Cardiac Magnetic Resonance Imaging Findings in a Cohort of Adolescents with Post-Coronavirus Disease 2019 mRNA Vaccine Myopericarditis. The Journal of Pediatrics.
- 14 – Patone et al. (2022) Risk of Myocarditis After Sequential Doses of COVID-19 Vaccine and SARS-CoV-2 Infection by Age and Sex. Circulation.
- 15 – Zheng et al. (2022) Real-world effectiveness of COVID-19 vaccines: a literature review and meta-analysis. International Journal of Infectious Diseases.
- 16 – Andrews et al. (2022) Effectiveness of COVID-19 booster vaccines against COVID-19-related symptoms, hospitalization and death in England. Nature medicine.
- 17 – Ioannou et al. (2021) COVID-19 Vaccination Effectiveness Against Infection or Death in a National U.S. Health Care System. Annals of Internal Medicine.
- 18 – Sheikh et al. (2021) BNT162b2 and ChAdOx1 nCoV-19 Vaccine Effectiveness against Death from the Delta Variant. The New England Journal of Medicine.
- 19 – Cohn et al. (2021) SARS-CoV-2 vaccine protection and deaths among US veterans during 2021. Science.
- 20 – Watson et al. (2022) Global impact of the first year of COVID-19 vaccination: a mathematical modelling study. Lancet Infectious Diseases.
- 21 – Xu et al. (2021) COVID-19 Vaccination and Non–COVID-19 Mortality Risk — Seven Integrated Health Care Organizations, United States, December 14, 2020–July 31, 2021. Morbidity and Mortality Weekly Report.
- 22 – Brownson et al. (2009) Evidence-Based Public Health: A Fundamental Concept for Public Health Practice. Annual Review of Public Health.