- Health
What you need to know about the current monkeypox outbreak: transmission, symptoms, treatments, etc.
Photo by CDC/Cynthia S. Goldsmith at Public Health Image Library (PHIL)
The ongoing monkeypox virus outbreak began in May 2022, when the U.K. notified the World Health Organization (WHO) of a handful of confirmed cases of monkeypox. Soon, cases appeared in many other countries, and as of 9 August 2022, there have been over 40,000 confirmed cases in 94 countries, with the vast majority of confirmed cases (40,012) occurring in countries that haven’t historically reported monkeypox. Due to the rapid increase in case numbers, the WHO determined that the multi-country monkeypox virus outbreak was a Public Health Emergency of International Concern (PHEIC) on 23 July 2022; a PHEIC is defined as “an extraordinary event which is determined to constitute a public health risk to other States through the international spread of disease and to potentially require a coordinated international response”.
Unlike the COVID-19 pandemic, which was caused by a previously unknown virus (SARS-CoV-2), scientists have known about the monkeypox virus since 1958. Therefore, much about the way this virus spreads and the symptoms of the disease it causes is already known. This previous knowledge, however, hasn’t kept disinformation and conspiracy theories about monkeypox from appearing on social media.
To clear up misconceptions about monkeypox virus and the current outbreak, Health Feedback will continue to update this explainer as we learn more about monkeypox.
Contents
- What is the monkeypox virus? First descriptions, animal hosts, human cases
- How is monkeypox transmitted among humans?
- What symptoms to look out for and how is monkeypox diagnosed?
- What monkeypox vaccines are available?
- What treatments are available for monkeypox?
- How dangerous is monkeypox?
<a Id="p1"></a>what Is The Monkeypox Virus? First Descriptions, Animal Hosts, Human Cases
<a Id="p1"></a>what Is The Monkeypox Virus? First Descriptions, Animal Hosts, Human Cases
The monkeypox virus is a viral zoonosis, meaning the disease is caused by a virus that is transmitted to humans from animals. Once in humans, the virus can spread via human-to-human transmission. Monkeypox virus is a member of the Orthopoxvirus genus, and other members of this genus include variola virus, which causes smallpox, and cowpox virus.
The monkeypox virus was first recognized in 1959 when Acta Pathologica Microbiologica Scandinavica, a monthly medical journal now known as APMIS, published a report about outbreaks of monkeypox that occurred among captive monkeys (Cynolmolgus monkeys) kept at the Statens Serum Institut in Copenhagen, Denmark, in 1958[1].
Despite its name, the animal reservoir of the monkeypox virus is likely not monkeys. While the definite animal reservoir remains unknown, evidence suggests that small mammals, such as squirrels and rats, play an important role in keeping the virus circulating. For instance, in a 2003 multi-state outbreak of monkeypox in the U.S., all cases of monkeypox occurred in people who had contact with pet prairie dogs that had been housed near to small mammals imported from Ghana, some of which were infected with the monkeypox virus.
In 1970, a 9-month old child suspected of having smallpox in the Democratic Republic of Congo, Africa, was the first recognized case of monkeypox virus infection in humans[2]. Due to the suspicion of smallpox, a related but different disease, specimens from the child were sent to the WHO Smallpox Reference Center in Moscow, Russia, where the virus was isolated and recognized as monkeypox.
According to the WHO, since 1970, 11 countries in west and central Africa have reported human cases of monkeypox. Additional but sporadic human cases have also been reported in countries outside west and central Africa since 2003, in people who had recently traveled to areas where monkeypox is endemic or who had contact with infected animals[3]. A disease is considered endemic if it’s consistently present in a specific area, and monkeypox is considered endemic in Benin, Cameroon, the Central African Republic, the Democratic Republic of the Congo, Gabon, Ghana (identified in animals only before this outbreak), Ivory Coast, Liberia, Nigeria, the Republic of the Congo, Sierra Leone, and South Sudan.
What makes the current monkeypox outbreak different is that the majority of confirmed cases in non-endemic countries have no history of travel to areas where monkeypox is endemic. While the first monkeypox case confirmed on 7 May 2022 in England occurred in an individual who had recently traveled to England from Nigeria, where the infection was believed to have happened, subsequent cases reported in England in May 2022 had “no link to travel to a country where monkeypox is endemic” and the same is happening in other non-endemic countries. This means that new cases of monkeypox are due to human-to-human transmission in countries that haven’t historically reported monkeypox.
How Is Monkeypox Transmitted Among Humans?
How Is Monkeypox Transmitted Among Humans?
Human-to-human transmission of the monkeypox virus can occur via a few routes: there is direct skin-to-skin contact with the monkeypox rash or lesions; indirect contact with objects, fabrics (including bedding and clothes), and surfaces contaminated with the virus; and contact with respiratory secretions.
While all of these are possible routes of transmission, the risk of infection varies with each form of transmission. In the current monkeypox outbreak, close physical contact during sexual activity appears to be the primary mode of transmission, particularly between men who have sex with men (MSM) in non-endemic countries. “For the most part this has been stable overtime, that the outbreak has been almost exclusively in men who have sex with men,” Boris Pavlin, an epidemiologist at the WHO’s Emerging Diseases Surveillance and Response, said during a WHO webinar about the outbreak on 27 July 2022.
This trend is borne out in the data. A study published in the New England Journal of Medicine (NEJM) on 21 July 2022, investigated 528 confirmed cases of monkeypox in 16 countries and found that 98% of individuals with the infection were gay or bisexual, and that in 95% of cases “transmission was suspected to have occurred through sexual activity”[4]. Case profile data from the WHO, released on in 16 August 2022 report, found a similar trend: for the cases where detailed information was available, 97.2% (8,382/8,627) of infections were in persons who identified as MSM, and in 91.0% (5,585/6,131) of cases transmission occurred during a sexual encounter.
In their report, the WHO noted that “separating transmission via skin-to-skin contact during sex and transmission via bodily fluids is not [emphasis theirs] possible”. This is because, even though skin-to-skin transmission during sexual activity is the primary mode of transmission, researchers are still investigating whether the virus can be spread by semen, vaginal fluids, urine and feces.
A study of samples from 12 monkeypox patients in Barcelona, Spain detected viral DNA in saliva, semen, urine and feces samples[5]. However, detecting viral DNA doesn’t mean that there’s infectious virus in these bodily fluids. So far, there has been a single report of infectious virus isolated in a semen sample taken in the early phase of infection (day six after symptom onset) from a monkeypox patient in Italy, with the authors noting that further studies are needed to better understand the “potential role of semen-driven transmission in the spreading of monkeypox infection”[6].
The same WHO data from 16 August 2022 also shows that, so far, other forms of transmission, such as indirect contact via contaminated objects or respiratory droplets, haven’t been major contributors of monkeypox transmission. According to WHO data from 6,131 monkeypox cases for which transmission data was available, transmission was due to a sexual encounter in 5,585 cases (91.0%), person-to-person in 409 cases (6.7%), other in 127 cases (2.1%), and contact with contaminated material in 10 cases (0.2%). This suggests that while nonsexual routes of monkeypox transmission can and do occur, they’re rare.
It’s important to note that anyone can become infected with monkeypox, and though at the moment, the majority of cases in non-endemic countries are in MSM and the primary mode of transmission is sexual contact, this could change. In a 22 July 2022 episode of the WHO’s Science in 5 webseries, WHO adviser Andy Seale said that while current efforts to stop the outbreak are focused on gay, bisexual men and other MSM, “we’re also keeping a strong eye on the data to see whether the outbreak will evolve into other communities”.
It should also be highlighted that, for African researchers who have dealt with monkeypox, information about transmission via sexual contact is not surprising. Evidence that monkeypox could spread via sexual activity had already been observed during the large and ongoing monkeypox outbreak that began in 2017 in Nigeria. In a 2019 scientific paper about the 2017 outbreak by Ogoina et al., the authors pointed out that “although the role of sexual transmission of human monkeypox isn’t established, sexual transmission is plausible in some of these patients through close skin-to-skin contact during sexual intercourse”[7].
Why is monkeypox primarily impacting MSM?
Monkeypox can occur in anyone, but as mentioned before in this explainer, the preponderance of cases so far have occurred in gay, bisexual and other men who have sex with men (MSM), leading to questions of why this is the case.
Kevin Woodward, an infectious disease specialist at McMaster University, told the Canadian Broadcast Corporation that monkeypox primarily hitting the queer community is an issue of bad luck. The first cases of monkeypox outside endemic countries have been in gay men, “and then primarily it’s being passed from person-to-person within those sexual networks,” explained Woodward. “Anyone can catch monkeypox, it’s spread through skin-to-skin contact, but it’s just because it has emerged first in that community, and that’s where some of the epidemiology lies right now”.
In this outbreak, sexual activity has played a large role in the transmission of monkeypox. Although sexual networks among MSM aren’t different from networks in other communities, there is a core group of MSM that is more densely connected, Kai Kupferschmidt reported for Nature. Early data from the outbreak suggests that the interconnected sexual networks of MSM have lead to a spread of monkeypox primarily in this community, but as has happened with other disease outbreaks, the disease could spread to other communities.
Recent debates about monkeypox transmission
Two debates related to monkeypox transmission have occurred, one over whether monkeypox should be considered a sexually transmitted infection (STI) and another over whether monkeypox is airborne. We’ll break down both of these debates below.
STIs are infections transmitted from one person to another predominantly via sexual contact; transmission can involve vaginal, oral or anal sex, as well as intimate skin-to-skin contact. Due to the preponderance of transmissions occurring via sexual contact, this has led to a debate over whether monkeypox should be considered an STI or not.
Most experts appear to agree that while monkeypox is not an STI, it is behaving like one in this outbreak. John Thornhill, one of the authors of the NEJM study that evaluated 528 cases of monkeypox and a clinical academic at Queen Mary University of London, said in a press release about the study that “it is important to stress that monkeypox is not a sexually transmitted infection in the traditional sense; it can be acquired through any kind of close physical contact. However, our work suggests that most transmissions so far have been related to sexual activity”[4].
The second debate over whether monkeypox is “airborne” appears to stem from a conflation of “airborne transmission” and “respiratory secretions”; Health Feedback has addressed the difference between these two terms in a previous claim review. In a 9 June 2022 statement, the U.S. Centers for Disease Control and Prevention (CDC) distinguished the two thusly:
“There are important differences between airborne transmission and transmission via respiratory secretions. Airborne transmission occurs when small virus particles become suspended in the air and can stay there for periods of time. These particles can spread on air currents, or sometimes even infect people who enter a room after the infected person has left. In contrast, monkeypox may be found in droplets like saliva or respiratory secretions that drop out of the air quickly. Long range (e.g., airborne) transmission of monkeypox has not been reported.”
As such, while transmission via respiratory secretions can happen, this type of transmission usually requires face-to-face proximity. People at a higher risk for this form of transmission include health care workers, members of the same household, and close contacts.
What Symptoms To Look Out For And How Is Monkeypox Diagnosed?
What Symptoms To Look Out For And How Is Monkeypox Diagnosed?
While the blister-like rash is the most notable symptom of monkeypox infection, the infection is often accompanied by general symptoms that occur with other viral infections like the flu. These can include fever, chills, swollen lymph nodes, muscle, back and joint pain, headaches, and exhaustion. The virus’ incubation period can last from 3 to 21 days, during which there are no symptoms, and symptoms can last from two to four weeks.
The monkeypox rash and lesions appear one to five days after the fever, have a distinct look, and progress through typical phases, although lesions in different stages can appear at the same time. However, the timeline of each phase and the size of the lesions can vary. The progression of the lesions looks like this:
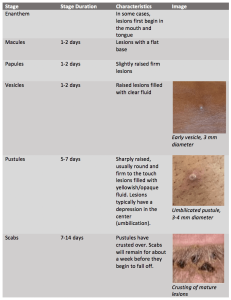
Sources: CDC, WHO, UK Health Security Agency. Image Credit: UK Health Security Agency.
As the outbreak progresses, knowledge about monkeypox’s symptomatology has progressed with it. The NEJM study by Thornhill et al. mentioned in the previous section, also looked at manifestations of monkeypox in the 528 cases, finding a number of symptoms not previously listed in case definitions of monkeypox[4]. For instance, the study found that while skin lesions occurred in 95% of cases, the number of skin lesions varied widely. In those with skin lesions, the majority had fewer than 10 lesions and 54 persons had only a single genital ulcer.
“We have shown that the current international case definitions need to be expanded to add symptoms that are not currently included, such as sores in the mouth, on the anal mucosa and single ulcers,” said Chloe Orkin, a professor of HIV medicine at Queen Mary University of London and one of the study’s authors, in a university press release. “Expanding the case definition will help doctors more easily recognize the infection and so prevent people from passing it on.”
Individuals who develop symptoms of the disease and/or were a close contact of someone diagnosed with monkeypox should get tested for monkeypox. Testing involves swabbing two to three lesions, followed by a PCR test to detect the presence of the monkeypox virus. At the moment, there are no at-home tests for monkeypox and, because the test involves swabbing lesions, testing can only occur once the lesions appear; work is being done to develop tests that could detect monkeypox in other ways, such as in the saliva, but these tests aren’t available at the moment.
It’s important to make clear that diagnosing monkeypox requires a PCR test and because other diseases can cause similar rashes and skin lesions, it’s not possible to diagnose monkeypox from dermatological manifestations alone. There have been two instances where individuals on public transportation–one in Madrid, Spain and the other in New York City, U.S.–surreptitiously filmed or photographed other individuals with lesions, claiming these individuals had monkeypox on social media.
But in both cases, the individuals photographed or filmed had neurofibromatosis, a genetic condition that causes benign tumors in the nerves and other parts of the body, including skin. These two cases demonstrate that it’s not possible to diagnose someone as having monkeypox simply through skin lesions as many dermatological conditions, including acne, eczema, and plaque psoriasis, can cause similar rashes and lesions.
What Monkeypox Vaccines Are Available?
What Monkeypox Vaccines Are Available?
Currently, there are two vaccines that have been licensed in the U.S. that can be taken to prevent monkeypox: JYNNEOS, which has been licensed for both smallpox and monkeypox, and ACAM2000, which has been licensed for smallpox, but can be used against monkeypox under the U.S. Food and Drug Administration’s (FDA) Expanded Access investigational New Drug (IND) mechanism, which allows drug products to be used outside clinical trials as long as there’s informed consent.
JYNNEOS, produced by Bavarian Nordic, has been approved by both the U.S FDA (in 2019) and the European Medicines Agency (in 2013). JYNNEOS is an attenuated, live, non-replicating vaccine, meaning it carries a harmless version of vaccinia virus that cannot replicate in humans but is able to elicit an immune response against both smallpox and monkeypox.
ACAM2000, produced by Sanofi Pasteur Biologics Co, also uses live vaccinia virus, but the vaccine isn’t delivered in a shot. Instead, a two-pronged stainless steel needle is dipped in the vaccine solution and then pricks the skin in the upper arm several times. This creates a localized infection, including a blister at the vaccination site, which then dries up as a scab, and leaves a small scar after the scab falls off. Compared to JYNNEOS, ACAM2000 causes more side effects and has more contraindications. Moreover, because ACAM2000 introduces a vaccinia virus that can replicate to some degree, properly caring the vaccination site is important for preventing the virus at the vaccination site from infecting other parts of the body and other people.
While both of these vaccines are currently being given in the context of the monkeypox outbreak, the CDC has noted that:
Because there are limitations in our knowledge about the effectiveness of these vaccines in the current outbreak, people who are vaccinated should continue to take steps to protect themselves from infection by avoiding close, skin-to-skin contact, including intimate contact, with someone who has monkeypox.
Although both ACAM2000 and JYNNEOS can be taken to prevent monkeypox, access to these vaccines is not guaranteed due to short supplies, especially in the case of JYNNEOS. So far, only Canada, the U.S. and certain countries in Europe have placed orders and/or have access to JYNNEOS; the U.S. also has a national stockpile of over 100 million doses of ACAM2000. To spread out the limited supplies, countries like the U.K. and Canada, are giving a single dose of JYNNEOS instead of two, and on 8 August 2022, U.S. health officials authorized a plan to give people one-fifth of the usual dose of JYNNEOS, a move that has been criticized due to the limited amount of data supporting this decision.
In the rest of the world, access to vaccines is even more limited. According to information from 2016, the WHO has a physical stockpile of about 2.4 million doses of a smallpox vaccine that can be delivered by a two-pronged needle; there’s an additional pledged stockpile of 31 million doses held by France, Germany, Japan, New Zealand and the U.S. However, it’s unclear when or how the WHO will distribute vaccine doses, and it’s very possible that inequitable distribution of vaccines, with many low-income countries being shut out of access, will occur.
Are people who got the smallpox vaccines decades ago immune?
A few decades ago, before smallpox was declared eradicated in 1980, smallpox vaccination was routine and some individuals 40 years and older who received the smallpox vaccine have wondered whether they may be protected from monkeypox. Observational studies, which is a type of study where researchers measure an outcome but don’t attempt to affect the outcome (e.g., they don’t provide a treatment), have shown that vaccination against smallpox is about 85% effective in preventing monkeypox. However, this has only been shown for the first three to five years after inoculation. Immunity wanes over time, but while there’s no guarantee that persons who received the smallpox vaccine decades ago will be protected from monkeypox infection, “experts believe it would still protect against severe illness,” Katrine Wallace, an epidemiologist at the University of Illinois, Chicago, told Bloomberg.
What Treatments Are Available For Monkeypox?
What Treatments Are Available For Monkeypox?
Currently there are no monkeypox-specific treatments, with clinical care focused on alleviating symptoms, which can include pain that’s been described as “excruciating at times”, as well as managing potential complications and preventing long-term sequelae.
There is one promising treatment though: the antiviral tecovirimat that has been approved for treating smallpox by the U.S. FDA, even though its safety and efficacy in humans has not been established. As explained in a NEJM perspective by Sherwat et al., this is because tecovirimat was approved via the “Animal Rule”, which provides a pathway to approval for drugs that treat serious or life-threatening conditions where it wouldn’t be ethical or feasible to conduct efficacy studies in humans[8]. According to this rule, while safety is established in healthy human study volunteers, efficacy is evaluated in animal studies.
The U.S. National Institutes of Health (NIH) are now developing a U.S.-based randomized control study to evaluate the safety and efficacy of tecovirimat as a treatment for monkeypox and another randomized, placebo-control study of tecovirimat will be done in the Democratic Republic of Congo.
Tecovirimat interferes with a protein on the surface of the monkeypox virus, keeping it from replicating normally, thus slowing down the spread of the infection. A paper by Adler et al. published in The Lancet, described the clinical features and management of monkeypox in seven patients, one of whom received tecovirimat. This patient had a shorter duration of symptoms and viral shedding compared to the other six patients, but the authors noted that they “are unable to say whether this was a result of treatment with tecovirimat”[9].
Since the beginning of the monkeypox outbreak, the FDA has allowed tecovirimat to be used under an expanded access investigational new drug protocol and the U.K. has approved tecovirimat for the treatment of poxviruses, including smallpox and monkeypox. Tecovirimat has been authorized under “exceptional circumstances” for the treatment of smallpox, monkeypox, and cowpox by the European Medicines Agency (EMA) since January 2022.
Similar to the situation with the smallpox/monkeypox vaccines, approving or authorizing tecovirimat as a treatment for monkeypox doesn’t guarantee access to tecovirimat. In the U.S., for instance, access to tecovirimat is limited and doctors need to fill out extensive paperwork and request the drug from the government’s stockpile. Because it’s an investigational drug, patients also have to give informed consent in order to use tecovirimat.
How Dangerous Is Monkeypox?
How Dangerous Is Monkeypox?
There are two clades of monkeypox; clade I is more deadly, with a mortality rate of up to 10%, while clade II is milder and less deadly, with a mortality rate of up to 1%. Genetic data from monkeypox cases early in the outbreak showed that cases in both the U.S. and Europe were infected with clade II. Please be aware that on 17 August 2022, the WHO renamed the two monkeypox clades; clade I was formerly known as the Congo Basin clade and clade II was formerly known as the West African clade. News articles and research papers published before this change may be using the old names.
Though in many cases monkeypox is self-limiting—meaning it goes away on its own, without specific treatment— in rare instances, infections can lead to medical complications and even death. In late July 2022, three countries (Brazil, Spain, and India) reported the first monkeypox deaths in non-endemic countries. Fatality rates are higher in African countries, with health officials reporting more than 70 suspected monkeypox deaths so far this year, though this number is probably undercounted due to limited testing and surveillance capacity, infectious diseases physician Dimie Ogoina of the Niger Delta University, Nigeria, told Nature.
REFERENCES
- 1 – von Magnus et al. 1959. A pox-like diseases in cynomolgus monkeys. Acta Pathologica Microbiologica Scandinavica
- 2 – Ladnyj et al. 1972. A human infection caused by monkeypox virus in Basankusu Territory, Democratic Republic of Congo. Bulletin of the World Health Organization.
- 3 – Oladimeji et al. 2022. The paradigm shift in monkeypox epidemiology. Nature Africa.
- 4 – Thornhill et al. 2022. Monkeypox virus infection in humans across 16 countries – April-June 2022. New England Journal of Medicine.
- 5 – Peiró-Mestres et al. 2022. Frequent detection of monkeypox virus DNA in saliva, semen, and other clinical samples from 12 patients, Barcelona, Spain, May to June 2022. Eurosurveillance.
- 6 – Lapa et al. 2022. Monkeypox virus isolation from a semen sample collected in the early phase of infection in a patient with prolonged seminal viral shedding. The Lancet.
- 7 – Ogoina et al. 2019. The 2017 human monkeypox outbreak in Nigeria – Report of outbreak experience and response in the Niger Delta University Teaching Hospital, Bayelsa State, Nigeria. PloS One.
- 8 – Sherwat et al. 2022. Tecovirimat and the treatment of monkeypox – past, present and future considerations. New England Journal of Medicine.
- 9 – Adler et al. 2022. Clinical features and management of human monkeypox: a retrospective observational study in the UK. The Lancet.